Alternatives for Treatment of Facial Asymmetry by Condylar Hyperplasia: A Review
Erika Céspedes, Helen Pardo and Manuel Bravo
DOI10.21767/2469-2980.100049
Erika Céspedes*, Helen Pardo and Manuel Bravo
Deparment of Orthodontics, Universidad de Cuenca, Cuenca, Ecuador
- *Corresponding Author:
- Erika Céspedes
Faculty of Dentistry
Universidad de Cuenca
Av El Paraíso y Av 10 de Agosto, Cuenca, Ecuador
Tel: 074051000, Ext: 3217
E-mail: mcr_erika26@hotmail.com
Received Date: December 27, 2017; Accepted Date: January 11, 2018; Published Date: January 18, 2018
Citation: Céspedes E, Pardo H, Bravo M (2018) Alternatives for Treatment of Facial Asymmetry by Condylar Hyperplasia: A Review. J Orthod Endod 3:15. doi: 10.21767/2469-2980.100049
Abstract
The purpose of the present review was to describe the numerous alternatives for the treatment of facial asymmetry caused by condylar hyperplasia and compare the results obtained in both aesthetic and functional aspects. A search for articles published from 2002 to 2017 in the PubMed and Lilacs databases was realized. A total of 42 articles were selected according to the inclusion criteria, of which 32 were used for the study. The selection of the most appropriate treatment for condylar hyperplasia depends on factors such as the age of the patient, degree of deformity, osteoblastic activity of the condyle, etiology and functional limitations. The procedure of first choice when confirming active growth of the condyle will be condylectomy in combination with orthognathic surgery. Condylectomy is essential in the presence of joint problems and tumors. The treatment with condylectomy as well as orthodontic camouflage through the use of mini-implants can be considered in cases of mild asymmetry.
Keywords
Facial asymmetry; Condylar hyperplasia; Condylectomy; Treatment
Introduction
Condylar mandibular hyperplasia described by Robert Adams in 1836 as pathology of the Temporomandibular Joint (TMJ) that is characterized by excessive mandibular growth usually unilateral, the head or neck of the affected condyle is hypertrophic, but preserves their basic form. It can occur at any age and continue after the period of growth of the individual. It occurs predominantly in women. Its etiology is unknown, although various factors have been mentioned such as: neoplasia, hypervascularity, previous trauma, metabolic hyperactivity, post-trauma mandibular condyle hyper-modeling, infection, osteoarthritis, arthritis, hormonal alterations, abnormal condylar load, intrauterine changes, genetic and hereditary factors. It can affect the size and morphology of the jaw, indirectly alter the maxilla, cause the development of dentofacial deformities such as mandibular prognathism, unilateral elongation of the condyle, neck, branch and mandibular body, facial asymmetry, malocclusion and pain, which compromises not only the facial aesthetics of the patient, but also their function [1-10].
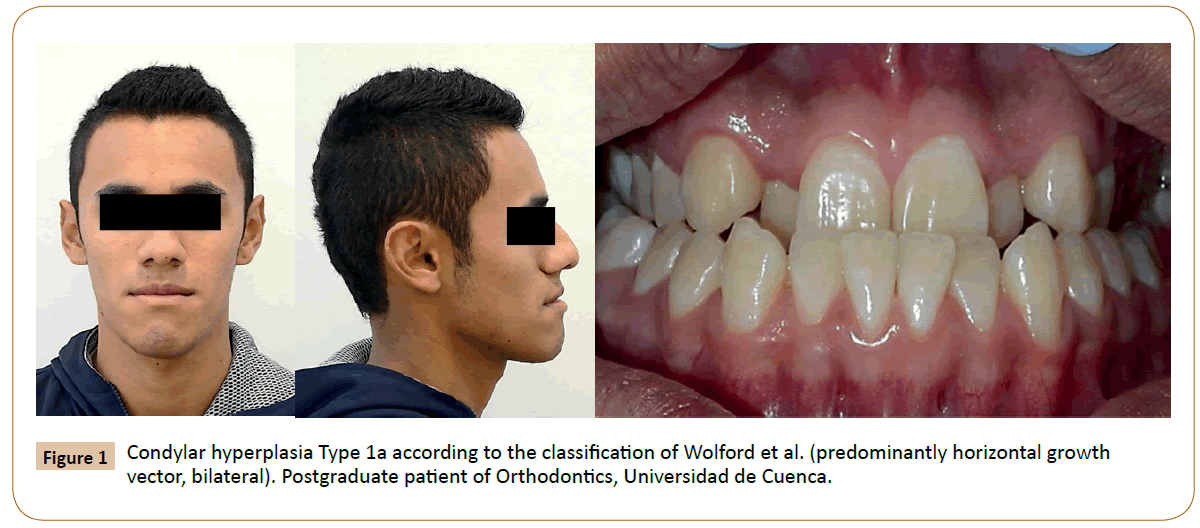
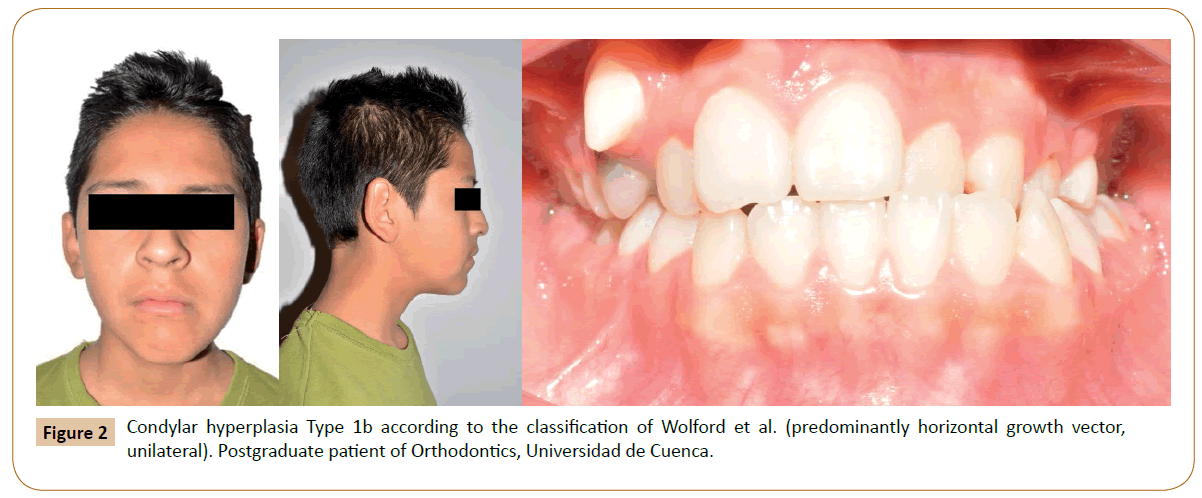
Some classifications of condylar hyperplasia have been proposed, in particular, Wolford et al. differentiate vertical or horizontal growth vectors that are usually related to specific condylar pathologies (Figures 1 and 2) [4,11].
During treatment planning, it is important to determine if the condyle is actively growing through a bone scan with technetium 99, which detects areas with increased osteoblastic activity [6]. In the literature, several therapeutic approaches are shown basically the procedures consist of condylectomy, orthognathic surgery, presurgical orthodontics, orthodontic camouflage or a combination of these. Since its management is the responsibility not only of the maxillofacial surgeon, but also of the orthodontist it is important that their work be combined in order to obtain a normal and functional occlusion in patients where it is directly affected by a base pathology, cellular hyperactivity in the condyle [12].
Although, a treatment protocol has been suggested based on the type of condylar hyperplasia [4], in general, there is no consensus on which the most appropriate management for these patients, so the need arises to perform this bibliographic review with the purpose of describing the different alternatives for the treatment of facial asymmetry caused by condylar hyperplasia and to compare the results obtained both in the aesthetic and functional aspects.
Materials and Methods
A bibliographic search was performed in the databases: PubMed and Lilacs, the terms used were: condylar hyperplasia, facial asymmetry, condylectomy, treatment. The inclusion criteria used for the selection of articles were:
1. Articles published from 2002-2017.
2. Articles in English, Spanish or Portuguese.
3. Systematic reviews.
4. Case-control studies.
5. Descriptive studies.
6. Case reports.
It is worth mentioning that an article published in 1991 was selected because it contained relevant information for the present review.
Results
The results of the search and the number of selected articles are shown in Table 1. A total of 42 articles were chosen according to the inclusion criteria, of which 32 were used in the present review, 8 studies were excluded as they provided irrelevant information on the types of treatment for condylar hyperplasia, 1 article was rejected because it was an expert opinion, and another article because facial asymmetry was not caused by condylar hyperplasia (Table 1).
| Database | Keywords | Results | Selected |
|---|---|---|---|
| PubMed | Facial asymmetry, condylar hyperplasia, condylectomy, treatment | 689 | 31 |
| Lilacs | Facial asymmetry, condylar hyperplasia, condylectomy, treatment | 397 | 11 |
| Total | 1086 | 42 |
Table 1: Search results of the databases.
The information obtained was classified based on the different treatment alternatives, as detailed below:
Orthognathic surgery
Kyteas et al. reported the case of a 32-year-old woman with condylar hyperplasia without active growth, facial asymmetry, maxilla canted to the right and chin deviation, treatment consisted in orthodontic and bimaxillary surgery that included LeFort I osteotomy and bilateral sagittal split osteotomy; finally, they observed a harmony in the facial profile and the occlusion [13]. Likewise, Thomé et al. presented the case of a 16-year-old patient with facial asymmetry caused by condylar hyperplasia. The scintigraphy showed a symmetric uptake in the condyles indicating that there was no hyperactivity. The patient underwent presurgical orthodontic preparation with unilateral maxillary intrusion with miniimplants and in the stage of final growth mandibular orthognathic surgery and genioplasty, without elimination of the condyle; the subsequent control was performed after one year, showing facial symmetry [14].
On the other hand, Wolford et al. compared a group of patients treated only with orthognathic surgery and another with high condylectomy combined with orthognathic surgery, a postoperative follow-up was performed after 5 years. All the patients from the first group relapsed to an occlusal and skeletal class III relationship that required a second intervention, while only one patient from the other group required a second surgery to correct a transverse recurrence of the maxilla while the mandible remained stable [15].
High and low condylectomy
Four studies addressed the treatment of condylar hyperplasia by condylectomy without orthognathic surgery. This procedure can be of two types: high condylectomy, if the upper part of the condyle is removed with a 3-5 mm dissection of the condylar head including the medial poles and lateral. Low condylectomy, when a total removal is performed usually at the level of the condyle-neck junction.
Roth et al. reported the case of a 14-year-old patient with laterognatism associated with an elongated right condylar neck, axial enlargement of the head of the right condyle and compensatory changes in the mandible, bone scan revealed increased activity of the right condyle. The patient's treatment consisted of high condylectomy with removal of 2.5 mm without orthognathic surgery, facial asymmetry was maintained [16].
Shankar et al. showed the case of a 36-year-old male patient with facial asymmetry, pain in the right condyle and feeding difficulties. He underwent high condylectomy with 10 mm of removal without orthognathic surgery because the authors report that facial symmetry was achieved. Although, postoperative evaluation photographs reveal that the asymmetry improved, it was not corrected in its entirety, yet condylectomy improved the function in the TMJ [17].
Pinto et al. presented the case of a 19-year-old patient with facial asymmetry, pain in the right TMJ that worsened with chewing and active condylar growth. She underwent a low condylectomy with 10 mm of removal and a protocol of functional exercises of the joint. Six months later, the facial asymmetry and the deviation of the lower dental midline decreased, as well as a slight open bite. The authors assert that the early treatment of condylar hyperplasia through condylectomy prevents the worsening of facial deformity, thus decreasing the need for orthognathic surgery [18].
Pulgar et al. reported twelve cases with condylar growth, of which seven showed facial asymmetry, one with ATM alteration and four the combination of both. The type of surgery performed varied according to the degree of severity of the condylar hyperplasia, in all patients a high condylectomy was performed, nine cases were managed only with condylectomy and three with orthognathic surgery that consisted in bilateral or unilateral sagittal split osteotomy, sometimes complemented by complete maxillary osteotomy and genioplasty. They carried out a follow-up of about 16 months, in all cases improvement in dental occlusion and facial symmetry with disappearance of the previous joint symptomatology was evidenced, no recurrence was observed [19].
Condylectomy in combination with orthognathic surgery
Nine articles address the treatment of patients with condylar hyperplasia through condylectomy combined with orthognathic surgery. Sheffer et al. published the case of a 34-year-old patient with condylar hyperplasia that presented a severe elongation in the left condyle. The treatment consisted of presurgical and postoperative orthodontics, high condylectomy with 10 mm removal, repositioning of the articular disc, orthognathic surgery with bilateral sagittal split osteotomy performed in a single surgical time [20].
Melo et al. evidenced the case of a 27-year-old patient with mandibular deviation and joint pain, bone scintigraphy revealed osteoblastic activity in the right condyle compatible with condylar hyperplasia. The treatment consisted of surgically assisted rapid palatal expansion, after 6 months high condylectomy was performed together with orthognathic surgery with maxillary impaction and mandibular repositioning. Five years after the treatment the patient presented a good facial appearance and absence of joint symptoms [21].
Silva et al. presented the case of a 22-year-old patient with joint pain and facial asymmetry compatible with condylar hyperplasia. The scintigraphy showed osteoblastic hyperactivity in the right condyle. After presurgical orthodontics, orthognathic surgery with maxillary impaction of 2 mm in the anterior and right side was performed; a maxillary rotation of 1.5 mm to the left for correction of the midline and later the condylectomy was performed. After six years, the patient presented a good general condition, without relapse of facial asymmetry or condylar hyperplasia [22].
Feldmann et al. reported the case of a 9-year-old patient diagnosed with right condyle hyperplasia. At the age of 11 years, the hyperplastic condyle was removed and a left sided oblique ramus osteotomy was performed. The postoperative orthodontic treatment allowed the growth to achieve a normalization of the occlusal relations, through the use of a Frankel type IV functional device. In the postsurgical control after two years, they observed a complete aesthetic and functional rehabilitation. The result remained stable 11 years after surgery [23].
Romero et al. described the case of a 13-year-old patient with condylar hyperplasia and active condylar growth. The treatment consisted of presurgical orthodontics and high condylectomy with 5 mm removal. After condylectomy the mandibular deviation had improved and the midlines were almost centered, but the asymmetry was still maintained, so that eleven months later the orthognathic surgery was executed, performing a Lefort I, bilateral sagittal split osteotomy and genioplasty, obtaining aesthetic results and favorable functional [8].
Porfirio et al. presented the case of a 37-year-old patient with facial asymmetry and active condylar growth. They performed the extirpation of the condyle. Three years later, the patient underwent orthognathic surgery with maxillary reposition and bone graft in the posterior region, left side advancement of the mandible and right side setback. The patient was managed with a two-phase protocol, since the authors indicate that in a single phase symptoms can occur at the level of the TMJ, in addition precise positioning of the condyle is needed. In post-surgical follow-up, occlusal and aesthetic symmetry were maintained [24].
Cerqueira et al. showed the case of a 26-year-old woman, at 13 she underwent a mandibular body osteotomy for correction of laterognatia, two years later she had evident relapse. The authors suspected the presence of a tumor at the level of the condyle, so the treatment consisted of orthodontic preparation, low condylectomy and LeFort I osteotomy [25].
Ribeiro et al. reported the case of a 48-year-old patient with facial asymmetry, difficulty speaking and chewing, pain in the TMJ and indefinite growth of the jaw. The therapeutic approach consisted of presurgical orthodontics, low condylectomy with removal of 8 mm due to the presence of an osteochondroma, reshaped of the condyle, disc repositioning, orthognathic surgery with mandibular setback and repositioning to the right and maxillary osteotomies for advancement and correction of the occlusal cant. In the postoperative follow-up after 6 months, stable results and facial symmetry were evidenced [26].
Thomé et al. presented a case with facial asymmetry caused by condylar hyperplasia where active condylar growth of the left condyle was confirmed. The patient underwent presurgical orthodontic preparation, orthognathic surgery (upper maxillary repositioning and reduction of body, ramus and gonial angle height) and high condylectomy with external access. The posterior control was performed after four years showing facial symmetry [15].
Orthodontic camouflage combined with condylectomy
Choi et al. presented as a treatment option a high condylectomy accompanied with orthodontic camouflage through mini-implants the upper molars of the affected side were intruded to improve the occlusal cant and the posterior open bite of the unaffected side. This combined treatment provided a satisfactory result without additional orthognathic surgery demonstrating that the molar intrusion can correct the occlusal cant and improve the facial asymmetry [27].
Discussion
Condylar hyperplasia is a complex pathology that requires a multidisciplinary approach. In literature several therapeutic options are described; however, the selection of the most appropriate treatment depends on many factors such as active growth of the condyle, severity of the disorder, age, etiology, joint symptomatology among others.
The single management by orthognathic surgery compromises the obtaining of a good occlusion; therefore, it is necessary to incorporate the orthodontic treatment to achieve optimal functional and aesthetic results. If condylar growth has finished, condylectomy can be excluded as reported by Kyteas et al. When the affectation is not very severe, mandibular surgery is performed, otherwise, bimaxillary. The techniques used have been unilateral osteotomy, bilateral osteotomy, genioplasty, Lefort I [8].
When condylar growth is active, condylectomy allows completely removing hyperplastic tissues and preventing the recurrence of the deformity, as presented by Wolford et al., Roth et al., Pinto et al., and Pulgar et al. Likewise, Shankar et al., Cerqueira et al. and Ribeiro et al. stated that with low condylectomy the results are predictable and stable because it allows to remove all remnants of fibrocartilage from the condyle, especially in those cases that present condylar hyperplasia due to a tumor (osteoma, osteochondroma). Although, some clinicians choose to wait for condylar growth to end to surgically treat the affected condyle, determining when that growth will finish is uncertain, on the other hand Olate et al. and Romero et al. suggest that condylectomy be performed as soon as possible in order to prevent facial deformity from getting worse. On the other hand, Sheffer et al. and Romero et al. recommend condylectomy even in those cases in which the condyle does not present active growth, but there is joint pain.
Shankar et al. and Roth et al. observed that in cases managed only with condylectomy, the occlusion and facial asymmetry improved, but this was not corrected in its entirety, whereas Pinto et al. achieved favorable changes in a case with removal of 10 mm of condyle without orthognathic surgery. This suggests that for the correction of facial asymmetry under this protocol a greater removal of the condyle is necessary. Contrarily, Pulgar et al. obtained success in all cases treated with condylectomy with and without orthognathic surgery, which is attributed to the appropriate selection of the treatment according to the degree of severity of the pathology. Therefore, in some cases it is expected that this single procedure avoids the need for additional surgical interventions, in others, as pointed out by Thomé et al. it will be appropriate to choose orthognathic surgery to correct any residual occlusal and facial asymmetry.
Other authors suggest the combination of orthodontics, orthognathic surgery and condylectomy to achieve a satisfactory and stable aesthetic over time [8,15,20-26], such surgical procedures could be performed simultaneously or in deferred form [21], according to this Porfirio et al. recommend following a two-phase protocol especially in cases of TMJ abnormalities with facial asymmetry to achieve accurate placement of the distal and proximal part of the condyle; otherwise, it may not improve the joint symptomatology or even generate it. The authors also clarify that performing the two procedures in a single intervention will depend on the surgeon's experience. In contrast, there are those who affirm that condylectomy and surgery performed in a single phase can help eliminate TMJ symptoms [12,19,20,22,26].
A different treatment approach for those cases of mild facial asymmetry is offered by Choi et al., a high condylectomy complemented with orthodontic camouflage that includes the intrusion of molars, the aesthetic and functional results obtained were favorable, unlike Shankar et al. and Roth et al. whose patients did not show a total correction of the asymmetry given the severity of it. Thus, exclude the orthognathic surgery to opt only for condylectomy and camouflage requires a thorough evaluation of the degree of facial deformity and the amount of molar intrusion in order not to compromise the aesthetics and stability of the results.
Another alternative to achieve symmetrical changes has been proposed by Thomé et al. combine orthodontic camouflage in the maxilla with mandibular orthognathic surgery without condylectomy since there was no active growth of the condyle.
Unfortunately, the scientific evidence currently available about the treatment of patients with condylar hyperplasia is limited and the few existing literature mostly shows case reports. Additional studies with a higher level of evidence are needed to determine which treatment is the most successful in the long term, identify which is the cause of condylar hyperplasia and the level of osteoblastic activity as well as establish treatment protocols. It would also be interesting to carry out future studies to assess the long-term stability of orthodontic camouflage performed by mini-implants.
Conclusions
1. The selection of the most appropriate treatment for condylar hyperplasia depends on factors such as the age of the patient, the degree of deformity, the osteoblastic activity of the condyle, the etiology and the functional limitations.
2. The treatment of first choice when confirming an active growth of the condyle will be condylectomy in combination with orthognathic surgery. In the absence of active growth of the condyle, the approach will be through orthognathic surgery.
3. In the presence of joint problems and tumors, condylectomy will be essential.
4. The single treatment with condylectomy can be considered in cases of mild asymmetry. If this procedure is chosen in more severe cases, a greater condyle excision may be necessary.
5. Orthodontic camouflage through the use of mini-implants is a good treatment option in cases of mild asymmetry.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Adams R. The disease in the temporomandibular articulation or joint of the lower jaw. In: A treatise on rheumatic gout or chronic rheumatic arthritis of all the joints. 2nd ed, London: Churchill, 1873: 271.
- Olate S, Moraes M (2012) Deformidad facial asimétrica. Papel de la hiperplasia condilar. Int J Odontostomat 6: 337-347.
- Billet M, Cadre B (2013) Condylar Hyperplasia. J Dentofacial Anom Orthod 16: 1-19.
- Wolford L, Mohabed R, Pérez D (2014) A classification system for conditions causing condylar hyperplasia. J Oral Maxillofac Surg 72: 567-595.
- Raijmakers P, Karssemakers L, Tuinzing D (2012) Female predominance and effect of gender on unilateral condylar hyperplasia: A review and meta-analysis. J Oral Maxillofac Surg 70: 72-76.
- Almeida L, Zacharias J, Pierce S (2005) Condylar hyperplasia: An updated review of literature. Korean J Orthod 45: 333-340.
- Nitzan DW, Katsnelson A, Bermanis I, Brin I, Casap N (2008) The clinical characteristics of condylar hyperplasia: experience with 61 patients. J Oral Maxillofac Surg 66: 312-318.
- Romero M, López V, Bravo L (2005) Tratamiento quirúrgico ortodóncico de la hiperplasia condílea: a propósito de un caso. Ortho Esp 45: 238-244.
- Uchoa Vasconcelos AC, Silveira FM, Etges A, Chaves Tarquinio SB (2015) Unilateral condylar hyperplasia: Evaluation of 6 cases. Clin Lab Res Den 21: 36-43.
- Wolford LM, Morale-Ryan CA, García-Morales P, Perez D (2009) Surgical management of mandibular condylar hyperplasia type 1. Proc (Bayl Univ Med Cent) 22(4): 321-329.
- Obwegeser HL, Makek MS (1986) Hemimandibular hyperplasia-hemimandibular elongation. J Maxillofac Surg 14: 183-208.
- López D, Corral C (2015) Hiperplasia condilar: características, manifestaciones, diagnóstico y tratamiento. Revisión de tema. Rev Fac Odontol Univ Antioq 26: 425-446.
- Kyteas P, McKensie S, Waite P, Kau Ch (2017) Comprehensive treatment approach for condylar hyperplasia and mandibular crowding with custom lingual braces and 2-jaw surgery. Am J Orthod Dentofacial Orthop 151: 174-185.
- Thomé M, Almeida R, Motta R, Mayrink G, Sanches A (2010) Condylar hyperactivity: diagnosis and treatment - case reports. Dental Press J Orthod 15: 77-83.
- Wolford LM, Mehra P, Reiche-Fischel O, Morales CA, García-Morales P (2002) Efficacy of high condylectomy for management of condilar hyperplasia. Am J Orthod Dentofacial Orthop 121: 136-151.
- Roth L, Biondi G, Azevedo R, Cerqueira A (2009) Hiperplasia condilar considerações sobre o tratamento e relato de caso. Rev. Cir. Traumatol. Buco-Maxilo-fac 9: 67-74.
- Shankar U, Chandra S, Krishnam R, Anitha G, Venkata K, et al. (2012) Condylar Hyperplasia. J Contemp Dent Pract 13: 914-917.
- Pinto I, Fonseca J, Vinagre A, Ángelo D, Sanz D, et al. (2016) Mandibular condylar hyperplasia: Diagnosis and management. Rev Dor São Paulo 17: 307-311.
- Pulgar D, Goñi I, Reinoso C (2015) Hiperplasia de cóndilo mandibular Reporte de doce casos. Rev. Otorrinolaringol. Cir Cabeza Cuello 75: 27-34.
- Sheffer M, Corso A, Tomazi M, Bortoluzzi M (2008) Condylar hyperplasia treated by simultaneous orthognathic surgery and high condylectomy. Rev Odonto Ciênc 23: 407-410.
- Melo J, De Sousa T, Ferrerira A, Morais L, Araújo J, et al. (2013) Tratamento cirúrgico de assimetria facial associada ao alongamento hemimandibular: relato de caso. Rev Cir Traumatol Buco-Maxilo-Fac 13: 31-36.
- Silva M, Pereira V, Dias E, Gimenez C, Gabrielli M (2010) Tratamiento de la deformidad facial causada por la Hiperplasia Condilar relato de caso. Acta Odontológica Venezolana.
- Feldmann G, Linder S, Rindler A, Söderström U (1991) Orthodontic and surgical treatment of unilateral condylar hyperplasia during growth-a case report. Eur J Orthod 13: 143-148.
- Porfirio S, De Santana T, Silva E, Faria A, Verissimo F (2014) Two-Stage Treatment of Facial Asymmetry Caused by Unilateral Condylar Hyperplasia. Braz Dent J 25: 257-260.
- Cerqueira F, Pitombeira L, Lima E, Turatti E (2010) Hiperplasia condilar associada à recidiva de deformidade dentofacial. Rev Cir Traumatol Buco-Maxilo-Fac 10: 15-20.
- Ribeiro M, Tochetto B, Macarini J, Gomes E, González P (2016) Surgical treatment of condylar hyperplasia associated with dentofacial deformity: low condylectomy, articular disc repositioning and orthognathic surgery. Int J Odontostomat 10: 207-213.
- Choi Y, Lee S, Baek M, Kim J, Park Y (2015) Consecutive condylectomy and molar intrusion using temporary anchorage devices as an alternative for correcting facial asymmetry with condylar hyperplasia. Am J Orthod Dentofacial Orthop 147: 109-121.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences