Developmental Disturbances In Permanent Teeth Due To Trauma To The Primary Dentition Orthodontic Endodontic Interdisciplinary Management: A Case Report And Literature. Review
Dr. Peter M. Di Fiore
Diplomate, American Board of Endodontics, Professor, Department of Endodontics, University of Texas, School of Dentistry, Houston, Texas, USA
- *Corresponding Author:
- Dr. Peter M. Di Fiore
Department of Endodontics, University of Texas, School of Dentistry
7500 Cambridge St. Ste. 6400, Houston, TX 77054, USA
Tel: +713-486-4227
E-mail: petermdifiore@aol.com
Received date: December 14, 2015, Accepted date: December 17, 2015, Published date: December 24, 2015
Citation: Di Fiore PM. Developmental Disturbances in Permanent Teeth due to Trauma to the Primary Dentition, Orthodontic – Endodontic Interdisciplinary Management: A Case Report and Literature Review. J Orthod Endod. 2015, 2:1.
Abstract
Background: Traumatic injuries to the primary dentition are a frequent occurrence in children during the preschool ages of 1 to 4 years and are primarily due to falls. Developmental disturbances to the permanent teeth can occur from trauma to the primary dentition, resulting in hypoplastic defects and disruptions in eruption. The aim of this clinical case report was to demonstrate that developmental disturbances in permanent teeth due to early trauma to primary teeth can have a favorable outcome with an interdisciplinary treatment approach. Methods: A clinical case is presented of the interdisciplinary management of a child with early trauma to the primary maxillary anterior dentition that resulted in the non-eruption of a maxillary permanent central incisor with enamel/dentin hypoplasia. A literature review is also presented on the incidence and prevalence of trauma to the primary dentition and its effects on the developing permanent teeth. Findings: Interdisciplinary management, with orthodontic, oral surgery and endodontic treatments in the clinical case presented, resulted in a favorable outcome for the maxillary anterior permanent dentition and the restoration and retention of the affected permanent tooth in a state of good health. Conclusions: Developmental disturbances to permanent teeth due to trauma to the primary dentition are usually detected well after the occurrence of the traumatic incident and in cases where multiple disturbances to the permanent teeth are identified an interdisciplinary treatment approach will often be necessary to achieve a favorable outcome.
Keywords
Trauma; Dental; Developmental; Disturbances
Introduction and Literature Review
The incidence and prevalence of pediatric traumatic dental injuries has been studied globally and especially in the Scandinavian countries of Denmark, Sweden and Norway, where public health dental care for children is easily accessed and epidemiological clinical data is readily available [1-6].
Traumatic injuries to the primary teeth are a frequent occurrence, however epidemiological reports on the incidence and prevalence of trauma to the deciduous dentition can vary depending upon the size, location and age range of the population sample studied [1-14].
Ravn, in a 7 year study of pediatric patients at the Royal College in Copenhagen Denmark, whose ages ranged from 9 months to 6 years, found that 165 children sustained traumatic injuries to 248 primary teeth [1]. Seventy-six percent were luxations that occurred between the ages of 1½ to 2½ years and later on followup examination, damage was observed to their permanent successors [1].
Andreasen and Ravn, in a retrospective review of the dental patient records of 487 preschool children in Copenhagen Denmark, found that 30% of the patients had sustained traumatic dental injuries to their primary dentition with the peak incidence occurring during the ages of 2 to 4 years [2]. Of the total 233 injured primary teeth, 69% were luxation type injuries, 20% were fracture type injuries, 7% were exarticulations, and the remaining 4% were undetermined injuries [2].
An extensive epidemiology study by Ravn conducted at the Copenhagen Municipal School Dental Service in Denmark which treated about 50,000 children each year, found that over a 5 year period, 9665 instances of traumatic injury events were reported in school children of 6 to 16 years of age that resulted in 11,767 injured teeth [3]. It was determined that 35% of boys and 23% of girls sustained a traumatic injury during their school age years [3].
Glendor, Halling, Andersson and Eilert-Petersson, in an epidemiological analysis of dental traumatic injuries in the county of Vastmanland Sweden with population of 62,914 children and adolescents, found that 1 out of every 91 individuals in the population had received treatment for traumatic dental injuries. However, among the 4702 preschool children 2 to 4 years of age in this population, 1 out of every 38 children received treatment for traumatic dental injuries [4].
Oldin, Lundgren, Nilsson, Noren and Robertson, in a recent multicenter longitudinal prospective/retrospective study in Gothenburg Sweden, covering a 5 year period from 2008 to 2012, found that the prevalence of traumatic dental injuries among 2326 children was 37.6%, largely due to falls of various kinds [5]. The overall yearly incidence of traumatic dental injuries for all children in the study was 2.8% and was highest at 4.7% among preschool children of 1 to 5 years of age and decreased with increasing age [5].
Skaare and Jacobsen, in a 1 year prospective study, in Buskerud County Oslo Norway, investigated the occurrence of traumatic injuries among a cohort of approximately 20,000 children of ages 1 to 8 years and found that the overall incidence of dental traumatic injuries was 1.3%, while the highest incidence of 2.5% occurred among children 3 to 4 years of age [6]. There were 477 injured primary teeth in 266 children, most of which were luxations of maxillary incisors primarily due to falls [6].
Schreiber, in an observational account over a 5 year period at Manchester Dental Hospital in England, found that 118 children sustained traumatic injuries to their primary anterior teeth which most commonly occurred during their toddler ages of 1½ to 2½years [7]. Among the injured children, 36% had their traumatized deciduous teeth extracted at the time of injury or shortly thereafter and 64%, who were followed every 6 months after injury, had retained their traumatized deciduous teeth until exfoliation [7].
Ferguson and Ripa examined preschool children over a 1 year period in the Head Start Program on Long Island New York and found that among 386 children whose ages ranged from 3 to 6 years, 114 children sustained traumatic dental injuries to their primary teeth at a prevalence 30% and among 61 children whose ages ranged from 4 to 5 years, 33 children sustained traumatic dental injuries at a prevalence of 54% [8]. Ninety-three percent of injures were in the maxillary arch and the maxillary central incisor was most frequently involved [8].
Meadow, Lindner and Needleman, in an investigation of oral trauma among patients as young as 13 months and as old as 19 years, who were treated at the Children’s Hospital Medical Center in Boston Massachusetts, reported that over a 1 year period 338 cases occurred in which 62% were due to falls and that while fracture injuries prevailed for permanent teeth, luxation injuries prevailed for primary teeth [9].
Garcia-Godoy et al. reported that during a five year period in a private pediatric dental center in Santo Domingo Dominican Republic, 114 children whose ages ranged from less than 1 year to 8 years, sustained trauma to 196 primary teeth during the ages of 1 to 4 years, of which 70% were luxation injuries due to falls [10].
Kenwood and Seow of Brisbane Australia, in a 3½ year retrospective investigation of pediatric dental records, reported that 43 children whose ages ranged from 15 months to 6 years with a mean age of 4 years, sustained traumatic dental injuries predominantly the result of falls or collisions [11]. Of the total 69 primary incisors that were injured, 9% had been loosened, 16% had been displaced, 29% had been fractured, 30% showed discoloration, and 16% had no signs [11].
Saporowski, Allred and Needleman, in a private pediatric dental practice in Boston, Massachusetts found that, among 222 children with a mean age of 3.8 years and a mean anterior overjet of 3 mm, 307 primary anterior teeth were traumatically luxated, of which 72% were due to falls [12]. Of the 307 injured teeth 60% were not treated but were observed, 22% were repositioned and 18% were extracted at the outset [12]. Of the 114 teeth that were followed for 4.3 years after injury, 55% did not develop any sequelae while 26% developed pulp necrosis, 11% developed pulp calcification and 8% became ankylosed [12].
Fried, Erickson, Schwartz and Keenan in a retrospective patient records audit at Montreal Children’s Hospital in Canada, of children whose ages ranged from 0.8 to 7.5 years with a mean age of 3.5 years, reported that 207 children had sustained subluxation injuries to their maxillary anterior primary incisors, of which 68% were due to falls, with the highest incidence occurring among children 1 to 4 years of age [13]. Periodic follow-up examinations that extended for 2 years after injury resulted in a low rate of morbidity and a high rate of normalcy with only 20% of the injured teeth extracted and 80% retained [13].
Eyuboglu, Yilmaz, Zehir and Sahin, in a 6-year retrospective review of the dental records of 13,480 children, aged 1 to 15 years, from Eastern Anatolia Turkey, found that 653 children had experienced dental trauma involving a total of 1021 [278 primary and 743 permanent] traumatized teeth [14]. The overall frequency of trauma for the sample population during the 6-year period was 4.9% [14]. The highest frequency of trauma occurred at age 5 for primary teeth and at age 10 for permanent teeth [14].
In summary the incidence of trauma to the primary dentition can be estimated to be about 5%, representing an occurrence rate, over a specific time period, of 1 traumatic injury for every 20 children [1,4,6,14] Whereas the prevalence, which is the measure of the occurrence of traumatic dental injuries among a population group can vary from about 30% to 50% [2,3,5,8] depending on the age range, size and location of the study sample. The age range at which trauma to the primary dentition most frequently occurs is between 1 to 4 years [1,2,4-8,10,13] with tooth luxation being the most common type of injury sustained [1,2,6,9,10,12,13], predominantly due to falls [5,6,9-13], and overwhelmingly affecting the maxillary primary incisors [8-14].
Traumatic injuries to the deciduous dentition can cause development disturbances in permanent teeth. In a systematic review of the literature conducted to determine the effects of traumatic injuries of the primary dentition on developing permanent teeth, evidence suggested that children with a prior history of trauma to their primary teeth had more developmental disorders to their permanent teeth than children without a history of prior traumatic injuries to their primary teeth [15]. Additionally, it was found that the severity of the developmental disorders of the permanent teeth were related to the severity of the traumatic injuries to the primary teeth, and that the younger the child at the time of the trauma to the primary teeth the more profound were the developmental disorders to the permanent teeth [15]. The types of disturbances that can occur to developing permanent teeth as sequelae to previous traumatic injuries to the primary teeth are: coronal discolorations and defects due to enamel hypoplasia and hypocalcification, crown and root dilacerations and malformations, arrested root formation, impaction, and premature, delayed or ectopic eruption [16].
A clinical and radiograph study by Andreasen and Ravn, of 103 school children in Copenhagen Denmark, who were observed up to 12 years after sustaining trauma to 213 primary anterior teeth between the ages 1 to 9 years, found that [88/213] 41% had developmental disturbances to their permanent teeth of which [75/88 ] 85% were enamel hypoplasia that manifested as yellowbrown coronal discolorations [17]. In another study that followed, the same investigators reported that of 487 Copenhagen school children with enamel hypoplasia of their permanent anterior teeth, [147/487] 30% had a history of trauma to their primary anterior teeth and [340/487] 70% did not. Among the children with a history of trauma to their primary anterior teeth, [85/147] 58% had enamel defects to their permanent teeth and among the children who did not have a history of trauma to their primary anterior teeth, [154/340] 45% had enamel defects to their permanent teeth, due to non-traumatic causes [18]. Therefore of all children with enamel hypoplasia of their permanent teeth, [85/340] 25% were the consequences of trauma to their primary teeth [18]. Two additional clinical and radiographic studies by Ravn, in Copenhagen Denmark that investigated the effects of intrusive luxation and exarticulation injuries of maxillary primary incisors, found that these severe types of traumatic injuries more often resulted in developmental disturbances to permanent teeth [19,20]. Among 78 pediatric patients who sustained 100 traumatic intrusions to their maxillary primary incisors the frequency of developmental disturbances to their permanent teeth was 54% [19], and among 77 pediatric patients who sustained 85 traumatic exarticulations of their maxillary primary incisors the frequency of developmental disturbances to their permanent teeth was 74% [20]. Although enamel hypoplasia was the most common defect observed it was found that the frequency and severity of the developmental disturbances to the permanent teeth increased when the trauma to the primary teeth occurred early at less than 3 years of age [19,20].
In a clinical case series of 16 children, who were referred to the Oral Surgery Department of Groningen University in the Netherlands for treatment of delayed eruption, dilaceration and malformation of their permanent incisors, van Gool found that 13 had a history of trauma to their primary dentition during the ages of 1 to 4 years [21].
In a 13 year retrospective investigation conducted at Kantonsspital in Lucerne Switzerland, that covered the treatment of 255 traumas to the primary teeth in 114 children whose ages ranged from 1 to 7 years, von Arx reported that the overall occurrence of developmental disturbances to the permanent teeth was [41/255] 16% with a higher frequency of [33/144] 23% occurring when primary incisors were fully erupted and a lower frequency of [8/111] 7% when they were not [22]. This finding indicated that the proximity of the apices of completely formed primary roots to developing permanent tooth buds at the time of trauma was a significant factor. The author also found that the most frequent developmental disturbances were enamel defects and discolorations at 68%, and dental deformations at 32%, most of which resulted when the primary tooth root was intruded [22].
A study by Sennhenn-Kirchner and Jacobs at the Center for Oral and Maxillofacial Diseases of the University of Goettingen in Germany involving 106 children who sustained trauma to 200 primary teeth during the ages of 1 to 8 years, found that among the 39 children, who were available for follow-up examination, 81 primary incisors had sustained traumatic injuries in which developmental damage was detected in 25% of their permanent successors with the highest frequency of 66% in children whose injuries occurred at 3 years or younger and were most frequently the result of intrusive luxations of their predecessors [23]. Among the 20 permanent teeth affected 10 had coronal hypoplastic defects, 5 had crown or root deformations, and 5 had irregular eruption [23].
In a clinical outcomes assessment, conducted by Altun, Cehreli, Guven and Acikel in Ankara Turkey, 78 pediatric patients who had originally presented at 1 to 2 years of age for treatment of intrusive luxations to 138 primary incisors were later examined at recall every 6 to 12 months for 7 years until complete eruption of the permanent successor occurred. It was reported that [36/138] 26% were initially extracted, [41/138] 30% were extracted because of post-traumatic consequences primarily due to pulp necrosis and [61/138] 44% were retained [24]. Recall examinations of their permanent successors at eruption revealed that [74/138] 54% had developmental disturbances that included enamel hypoplasia, crown or root deformation, and ectopic eruption [24].
In summary it was found that the prevalence of developmental disturbance to permanent teeth due to trauma to the primary dentition had a wide variance that ranged from 25% to 66% and was directly influenced by the severity of the injury [19-24] and the age of the patient at the time of injury [19-23]. The younger the child, [3 years or less], at the time of trauma to the primary dentition and the more severe the injury to the primary teeth [21-23], especially with intrusive luxations and exarticulations [19,20], the more frequent was the occurrence [22,23] and the more severe were the injuries [21-24] to the permanent teeth. The most common type of developmental disturbance found in permanent teeth due to trauma to the primary dentition were enamel/dentin hypoplastic defects [16-20,22-24], however, developmental dental deformaties and disruptions in eruption that included delayed, ectopic and unerupted permanent teeth, more often occurred with severe traumatic injuries to the primary dentition [16,19-24]
A clinical case report is presented of early trauma to the anterior maxillary primary dentition that resulted in noneruption and enamel/dentin hypoplasia of a permanent maxillary central incisor. Interdisciplinary management with oral surgery, orthodontic and endodontic treatments resulted in a favorable outcome for the maxillary anterior permanent dentition and restoration and retention of the affected tooth.
Case Report
History
The dental history as related by the mother was that her son at 5 years of age fell while riding his bicycle and hit the ground under his nose and on his front teeth. His maxillary primary central incisors were present at the time of the accident and later at 7 years of age after the primary central incisors had exfoliated, the permanent right central incisor began to erupt but the permanent left central incisor did not. After an unattended period of 3 years, the left central incisor had still not erupted and the patient now at 10 years of age and under orthodontic treatment, was referred by his orthodontist to an oral surgeon for surgical exposure of the un-erupted maxillary left central incisor to facilitate orthodontic extrusion. The interdental space between the right central incisor and left lateral incisor was orthodontically opened and orthodontic extrusion of the left central incisor commenced. Later after orthodontic extrusion had been accomplished, the left central incisor was fully visible orally and the full extent of the coronal developmental defect was observed by the orthodontist. The patient, at 12 years of age, was then referred for endodontic examination and treatment.
Examination
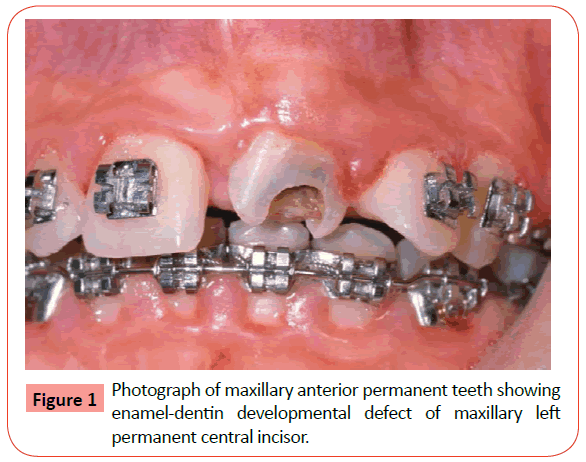
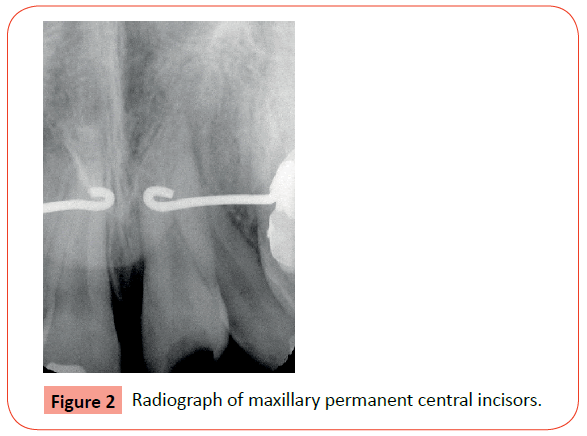
A 12 year old healthy boy with a non-significant medical history and no known allergies, who was currently under orthodontic treatment, was referred by his orthodontist for endodontic evaluation and treatment of his maxillary left permanent central incisor with a coronal enamel/dentin hypoplastic developmental defect. Upon clinical examination, the coronal defect encompassed the labial-lingual surfaces of the incisal portion of the tooth and was further complicated by deep caries with probable pulpal involvement [Figure 1]. Both the right and left central incisors were asymptomatic, not mobile, had intact gingival attachments and pulp tested within normal limits. The left lateral incisor presented with a severe labial inclination and distal rotation [Figure 1]. Radiographic examination showed that both central incisors were fully developed with normal appearing pulp chambers, pulp canals, root apices and periapices [Figure 2]. Radiographic examination also showed the extent of the coronal incisal defect on the left central incisor and the severe root angulation of the left lateral incisor [Figure 2].
Treatment
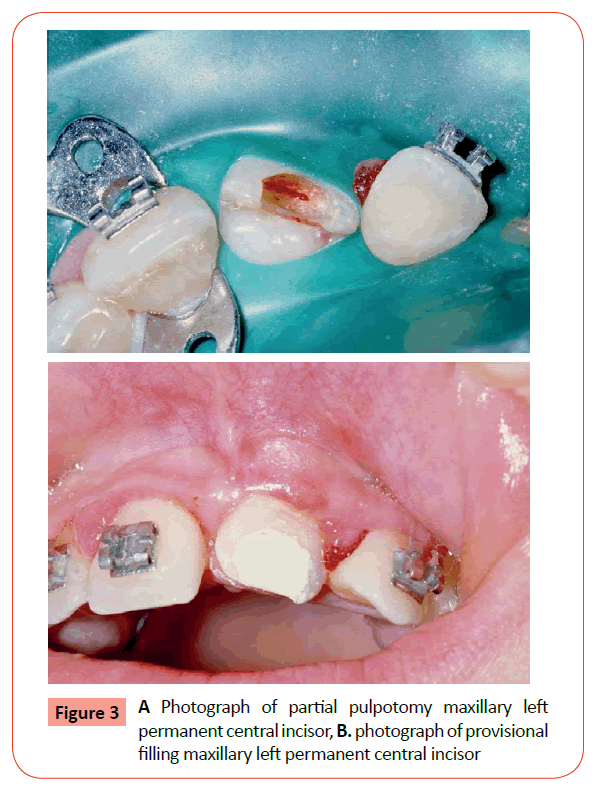
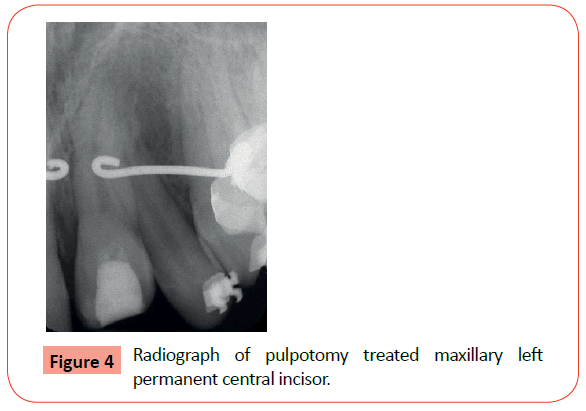
Local anesthesia was administered and the hypoplastic enamel/ dentin and carious dentin in the coronal incisal defect of the left maxillary central incisor was excavated under dental dam isolation. Exposure of the pulp was encountered and a partial pulpotomy 2 mm in depth was performed [Figure 3A]. A thick paste of calcium hydroxide USP and physiologic saline was applied to cover the exposed pulp and the coronal cavity was filled with glass ionomer as a provisional filling [Figure 3B]. A radiographic image of the tooth was then taken [Figure 4]. Three weeks later the tooth was restored with a composite resin and the patient was sent back to his orthodontist.
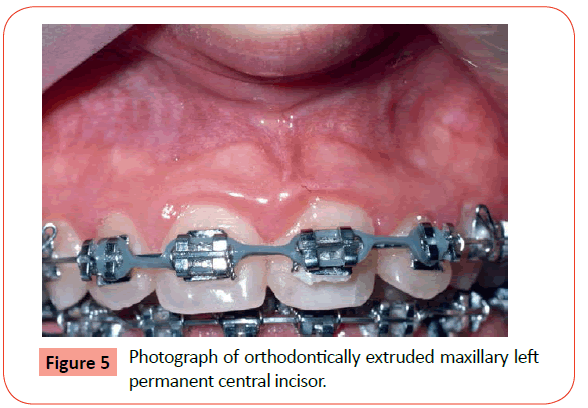
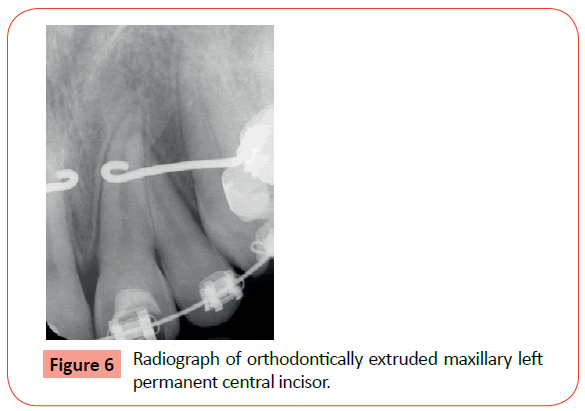
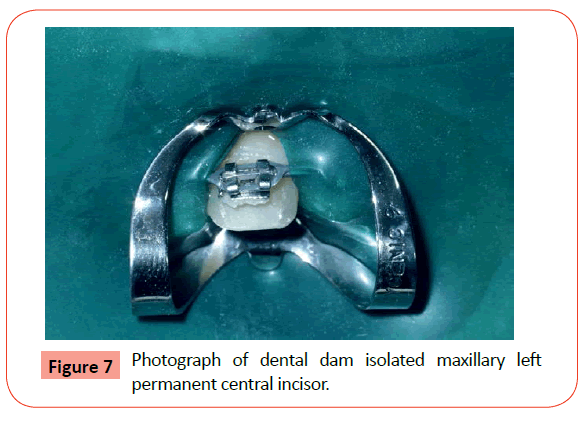
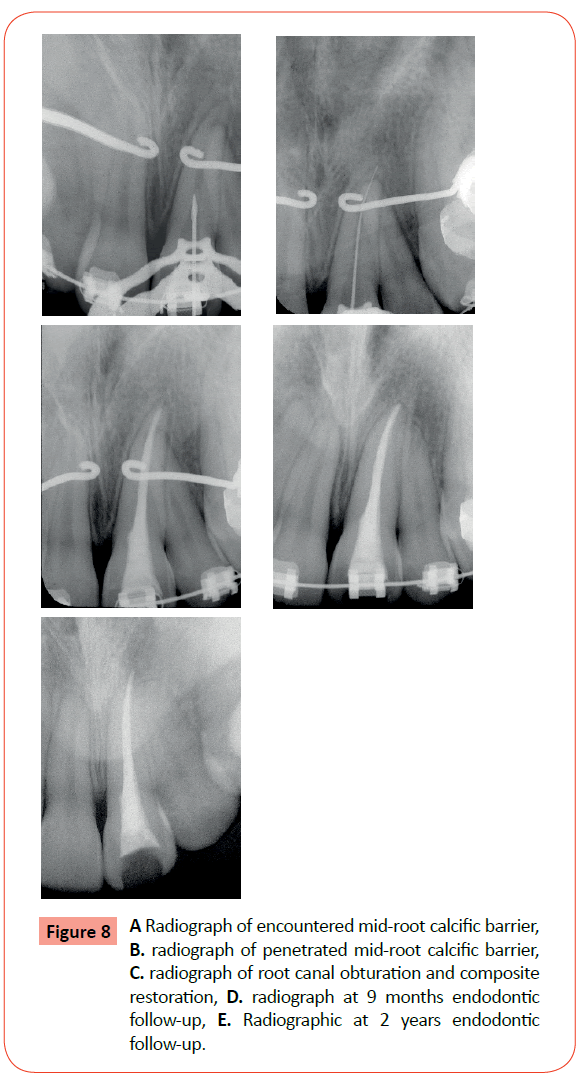
Nine months later when the maxillary left central incisor had been fully extruded and the anterior teeth were undergoing orthodontic movement [Figure 5], a radiograph of the left central incisor showed a mid-root calcific barrier and a normal periapex [Figure 6]. Percussion and palpation results were normal but pulp test results were inconclusive. A diagnosis of asymptomatic irreversible pulpitis with normal periapex was made. Local anesthesia was administered, dental dam isolation applied [Figure 7] and endodontic access accomplished. Upon root canal exploration the mid-root calcific barrier was encountered [Figure 8A] and penetrated to achieve working length measurement [Figure 8B]. Pulpal tissue was removed and the root canal was cleaned, shaped and prepared to a working length measurement of 26 mm and a master apical file size of 55, using hand and rotary instruments and obturated with gutta-percha and a calcium hydroxide based sealer. The access cavity was filled with a composite resin and a radiograph taken [Figure 8C]. The patient was then referred to his orthodontist to continue with orthodontic treatment.
Recalls
Nine months after completion of root canal treatment the patient was still undergoing orthodontic treatment and at examination all clinical findings were normal. Radiographic examination of the maxillary left central incisor showed a well filled root canal and normal appearing periapical and periradicular tissues [Figure 8D].
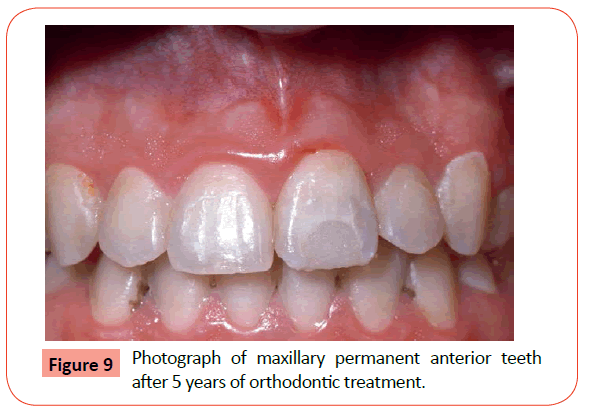
Two years after completion of root canal treatment, the patient had completed 5 years of orthodontic treatment at age 15 years. Radiographic examination showed a composite resin restored maxillary left central incisor with normal periapical and periradicular tissues and the right and left central incisors, and left lateral incisor with mild apical root resorption [Figure 8E]. Clinical examination revealed normal healthy maxillary anterior teeth in good orthodontic alignment and the restored maxillary left central incisor [Figure 9].
Discussion
In the case presented the original traumatic injury to the anterior maxillary dentition occurred at 5 years of age. Two years later at 7 years of age, at the time when the eruption of the maxillary permanent incisors would normally be observed, the maxillary right central and lateral incisors had begun to erupt but the left central incisor did not and the left lateral incisor was ectopically erupting in an abnormally excessive labial position. It is not unusual that discovery of developmental disturbances in eruption due to trauma to the primary dentition, often occurs well after the actual injury, at a time of when normal eruption of the permanent teeth would usually be anticipated [21-24].
After an unattended period of time, the patient, at 10 years of age, was referred to an oral surgeon by his attending orthodontist for surgical exposure of the unerupted maxillary left central incisor. Surgical exposure was achieved by reflecting a full thickness labial mucoperiosteal flap and exposing the crown of the unerupted maxillary left central incisor. An orthodontic bracket, pre-ligated with a 0.015 gauge wire, was bonded to the labial surface of the crown and the ligated wire from the bracket was attached to the arch wire of the orthodontic appliance that was already in place to open the space for extrusion of the left central incisor. The surgical flap was repositioned and sutured. After a period of 2 weeks to allow for surgical healing, elastic power chain traction was then applied to provide controlled simulated physiological eruptive occlusal movement of the tooth through the attached gingival tissues into a normal position within the maxillary anterior dental arch. Although, techniques to accomplish extrusion of unerupted teeth may vary, the surgical-orthodontic technique that was followed in this case was a standard treatment procedure for orthodontic extrusion of unerupted impacted maxillary anterior teeth [25-30].
After orthodontic extrusion was accomplished the full extent of the coronal developmental defect in enamel and dentin was visibly observed [Figure 1] and the patient was then referred for endodontic treatment because of probable pulpal involvement. Operative treatment commenced with complete excavation of the hypoplastic enamel and dentin and associated caries that revealed an exposure of the incisal pulp. A partial pulpotomy was performed [Figure 3A] with calcium hydroxide as the therapeutic agent to allow for the formation of a dentin-bridge, as originally described by Cvek [31], and a resin modified glass ionomer provisional filling was placed [Figure 3B]. Although full root length growth had already occurred, preservation of the pulp was important to allow for complete closure of the apical foramen [32], until such time as the tooth would be fully extruded into the maxillary anterior dental arch and root canal treatment could be expeditiously accomplished with proper dental dam isolation [33].
Orthodontic treatment continued and the patient was referred back, 9 months later, for root canal treatment of the maxillary left central incisor. Iatrogenic histological changes have been observed in the dental pulps of teeth after application of extrusive orthodontic forces [34-36]. Therefore it was reasonable to assume that the pulp in this partial pulpotomy treated maxillary central incisor could have become compromised and would be more susceptible to irreversible pulpal changes and possibly pulpal necrosis after the application of extrusive forces [33]. Pulp test results before initiation of root canal treatment were inconclusive and a mid-root calcific barrier was observed on radiographic examination [Figure 6]. Upon initiation of root canal treatment it was found that the pulpal tissue coronal to the mid-root calcific barrier had degenerated and the pulpal tissue apical to the mid-root calcific barrier appeared vital but inflamed. It may be speculated that the mid-root pulpal calcification, that was radiographically observed and clinically encountered, had provided a barrier, for a certain period of time that prevented the further degeneration of the apical portion of the pulp. Root canal treatment was completed without complications and recall examinations at 9 months and 2 years post treatment followed [Figures 8 A, B, C , D and E]. The patient then continued with orthodontic treatment.
At the first recall examination, 9 months after root canal treatment all clinical examination and radiographic findings [Figure 8D] were normal. At the second recall examination 2 years after root canal treatment, when orthodontic treatment had been completed at age 15 years, all clinical examination findings continued to be normal, and although there were mild apical root resorptions of the maxillary incisors, which are not unusual following orthodontic treatment [37-41], all other radiographic findings were normal [Figure 8E].
This patient, at the end of a case history period of 10 years, from age 5 years, when the initial dental trauma occurred, to age 15 years, when orthodontic treatment was completed, had a very favorable treatment outcome with good functional and esthetic alignment of his permanent anterior teeth [Figure 9], for which his parents were very pleased.
Conclusion
Traumatic injuries to the primary dentition are a relatively frequent event and subsequent developmental disturbances to the permanent teeth are not an uncommon occurrence. In the management of pediatric traumatic injuries to the primary teeth, careful follow-up examinations are necessary to identify emerging abnormal eruption patterns and malformations of their permanent successors and to coordinate an interdisciplinary treatment approach that will provide a favorable treatment outcome for the developing dentition of young patients.
References
- Ravn JJ (1968) Sequelae of acute mechanical traumata in the primary dentition. A clinical study.ASDC J Dent Child 35: 281-289.
- Andreasen JO, Ravn JJ (1972) Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample.Int J Oral Surg 1: 235-239.
- Ravn JJ (1974) Dental injuries in Copenhagen schoolchildren, school years 1967-1972.Community Dent Oral Epidemiol 2: 231-245.
- Glendor U, Halling A, Andersson L, Eilert-Petersson E (1996) Incidence of traumatic tooth injuries in children and adolescents in the county of Västmanland, Sweden.Swed Dent J 20: 15-28.
- Oldin A, Lundgren J, Nilsson M, Noren JG, Robertson A. (2015) Traumatic dental injuries among children aged 0–17 years in the BITA study – A longitudinal Swedish multicenter study. Dent Traumatol, 31: 9-17.
- Skaare AB, Jacobsen I (2005) Primary tooth injuries in Norwegian child ren (1-8 years).Dent Traumatol 21: 315-319.
- Schreiber DK. (1959) The effect of trauma on the anterior deciduous teeth. Brit Dent J 106:340-344.
- Ferguson FS, Ripa LW (1979) Prevalence and type of traumatic injuries to the anterior teeth of preschool children. J Pedod 4: 3-8.
- Meadow D, Lindner G, Needleman H (1984) Oral trauma in children.Pediatr Dent 6: 248-251.
- Garcia-Godoy F, Garcia-Godoy F, Garcia-Godoy FM (1987) Primary teeth traumatic injuries at a private pediatric dental center.Endod Dent Traumatol 3: 126-129.
- Kenwood M, Seow WK (1989) Sequelae of trauma to the primary dentition.J Pedod 13: 230-238.
- Soporowski NJ, Allred EN, Needleman HL (1994) Luxation injuries of primary anterior teeth--prognosis and related correlates.Pediatr Dent 16: 96-101.
- Fried I, Erickson P, Schwartz S, Keenan K (1996) Subluxation injuries of maxillary primary anterior teeth: epidemiology and prognosis of 207 traumatized teeth.Pediatr Dent 18: 145-151.
- Eyuboglu O, Yilmaz Y, Zehir C, Sahin H (2009) A 6-year investigation into types of dental trauma treated in a paediatric dentistry clinic in Eastern Anatolia region, Turkey.Dent Traumatol 25: 110-114.
- Lenzi MM, Alexandria AK, Ferreira DM, Maia LC (2015) Does trauma in the primary dentition cause sequelae in permanent successors? A systematic review.Dent Traumatol 31: 79-88.
- Andreasen JO, Sundström B, Ravn JJ (1971) The effect of traumatic injuries to primary teeth on their permanent successors. I. A clinical and histologic study of 117 injured permanent teeth.Scand J Dent Res 79: 219-283.
- Andreasen JO, Ravn JJ (1971) The effect of traumatic injuries to primary teeth on their permanent successors. II. A clinical and radiographic follow-up study of 213 teeth.Scand J Dent Res 79: 284-294.
- Andreasen JO, Ravin JJ (1973) Enamel changes in permanent teeth after trauma to their primary predecessors.Scand J Dent Res 81: 203-209.
- Ravn JJ (1976) Developmental disturbances in permanent teeth after intrusion of their primary predecessors.Scand J Dent Res 84: 137-141.
- Ravn JJ (1975) Developmental disturbances in permanent teeth after exarticulation of their primary predecessors.Scand J Dent Res 83: 131-134.
- von Gool AV (1973) Injury to the permanent tooth germ after trauma to the deciduous predecessor.Oral Surg Oral Med Oral Pathol 35: 2-12.
- von Arx T (1993) Developmental disturbances of permanent teeth following trauma to the primary dentition.Aust Dent J 38: 1-10.
- Sennhenn-Kirchner S, Jacobs HG (2006) Traumatic injuries to the primary dentition and effects on the permanent successors - a clinical follow-up study.Dent Traumatol 22: 237-241.
- Altun C, Cehreli ZC, Güven G, Acikel C (2009) Traumatic intrusion of primary teeth and its effects on the permanent successors: a clinical follow-up study.Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107: 493-498.
- Levine B, Skope L (1979) Direct bonding of unerupted teeth for orthodontic movement.J Am Dent Assoc 98: 55-57.
- Fifield CA Jr (1986) Surgery and orthodontic treatment for unerupted teeth.J Am Dent Assoc 113: 590-591.
- McDonald F, Yap WL (1986) The surgical exposure and application of direct traction of unerupted teeth.Am J Orthod 89: 331-340.
- Kocadereli I, Turgut MD (2005) Surgical and orthodontic treatment of an impacted permanent incisor: case report.Dent Traumatol 21: 234-239.
- Farronato G, Maspero C, Farronato D (2009) Orthodontic movement of a dilacerated maxillary incisor in mixed dentition treatment.Dent Traumatol 25: 451-456.
- Valladares Neto J, de Pinho Costa S, Estrela C (2010) Orthodontic-surgical-endodontic management of unerupted maxillary central incisor with distoangular root dilaceration.J Endod 36: 755-759.
- Cvek M (1978) A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture.J Endod 4: 232-237.
- MOORREES CF, FANNING EA, HUNT EE Jr (1963) AGE VARIATION OF FORMATION STAGES FOR TEN PERMANENT TEETH.J Dent Res 42: 1490-1502.
- Hamilton RS, Gutmann JL (1999) Endodontic-orthodontic relationships: a review of integrated treatment planning challenges.Int Endod J 32: 343-360.
- Mostafa YA, Iskander KG, El-Mangoury NH (1991) Iatrogenic pulpal reactions to orthodontic extrusion.Am J Orthod Dentofacial Orthop 99: 30-34.
- SÃbay RK, Kaya H, Tarim B, Sübay A, Cox CF (2001) Response of human pulpal tissue to orthodontic extrusive applications.J Endod 27: 508-511.
- Ramazanzadeh BA, Sahhafian AA, Mohtasham N, Hassanzadeh N, Jahanbin A, et al. (2009) Histological changes in human dental pulp following application of intrusive and extrusive orthodontic forces.J Oral Sci 51: 109-115.
- Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, et al. (1982) Root resorption after orthodontic treatment of traumatized teeth.Am J Orthod 82: 487-491.
- Levander E, Malmgren O (1988) Evaluation of the risk of root resorption during orthodontic treatment: a study of upper incisors.Eur J Orthod 10: 30-38.
- Mirabella AD, Artun J (1995) Risk factors for apical root resorption of maxillary anterior teeth in adult orthodontic patients.Am J Orthod Dentofacial Orthop 108: 48-55.
- Mirabella AD, Artun J (1995) Prevalence and severity of apical root resorption of maxillary anterior teeth in adult orthodontic patients.Eur J Orthod 17: 93-99.
- Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE (2010) Root resorption associated with orthodontic tooth movement: a systematic review.Am J Orthod Dentofacial Orthop 137: 462-476.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences