Endodonic - Orthodonic Interdisciplinary Management of Teeth Traumaized During Orthodonic Treatment: Case Reports
Peter M. Di Fiore
DOI10.21767/2469-2980.100025
Department of Endodontics, School of Dentistry, University of Texas, USA
- *Corresponding Author:
- Peter M. Di Fiore
Department of Endodontics, American Board of Endodontics Professor, School of Dentistry, University of Texas, Texas, USA
E-mail: petermdifiore@aol.com
Received date: May 15, 2016; Accepted date: May 27, 2016; Published date: June 02, 2016
Copyright: © 2016 Di Fiore PM, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Orthodontic treatment most often occurs during the preadolescent and adolescent years, a time when traumatic dental injuries are frequent. When orthodontic patients sustain dental trauma during active orthodontic treatment, endodontic assessment and treatment of the traumatized teeth are essential for continuation of orthodontic treatment.
Aim: The aim of this article is to present the endodontic treatment of two teenage orthodontic patients who sustained traumatic injuries to their maxillary permanent incisors while undergoing active orthodontic treatment.
Results: The endodontic/orthodontic interdisciplinary management of traumatized maxillary permanent incisors in two teenage orthodontic patients resulted in favorable endodontic treatment outcomes and normal progression of orthodontic treatment.
Conclusion: Successful endodontic treatment outcomes and resumption of orthodontic treatment can be achieved, for teenage orthodontic patients who sustain traumatic dental injuries to their permanent teeth during orthodontic treatment, when a close liaison exists between the endodontist and orthodontist.
Keywords
Trauma; Orthodontic; Patients; Endodontic; Treatment
Introducion
The prevalence of malocclusion and the definite need for orthodontic treatment among young patients in the United States has been investigated and substantiated by data from the National Centre for Health Statistics, National Health and Examination Surveys [1]. It has been reported that of the children surveyed 22.4% had a definite malocclusion and 14.2% hadsevere malocclusion [2]. It also has been reported that while 49% of preadolescent and adolescent children had little need for orthodontic treatment, 17.3% had a definite need for orthodontic treatment, and 33.7% had a probable need for orthodontic treatment [3,4]. The percentage of preadolescents and adolescents who received orthodontic treatment varied among different ethno-racial and socio-economic groups, however it was estimated that approximately 30% had received orthodontic treatment [1,5].
Traumatic dental injuries commonly occur in young patients during their preadolescent and adolescent years [6-14]. Although the prevalence of traumatic dental injuries in young patients may vary according to the specific patient population sampled, an average prevalence of 30% would be a realistic estimate based on investigations that individually reported prevalence findings of 19%, 34%, 31%, 30%, 66%, 30%, 15%, 38%, and 10% [6-14]
In an extensive literature review on the epidemiology of traumatic dental injuries it was found that there was a high prevalence of traumatic dental injuries throughout the world, and with some variations among different countries, one third of all preschool children and one fourth of all school children had sustained traumatic dental injuries to their anterior teeth [15]. Another extensive literature review on the etiology of traumatic dental injuries found that the major causes of traumatic dental injuries in children were due to accidental falls and collisions, and being struck during recreational activities [16].
Three contemporary comprehensive epidemiological investigations, of large population samples of children and adolescents, found that the incidence of traumatic dental injuries were 2.8%, 1.8%, and 2.2% [13,17,18]. The results of these investigations were quite similar and indicate that the anticipated chance of individuals in these age groups experiencing traumatic dental injuries would be about 2.4%.
With orthodontic treatment predominantly occurring during the preadolescent and adolescent years [1,5] and with traumatic dental injuries commonly occurring during these same years [6-14], it is understandable that orthodontic patients will likely sustain traumatic dental injuries to their anterior permanent dentition. In an investigation of 1367 orthodontic patients during a 5 year period, it was found that 10.3% of these patients sustained traumatic dental injuries to their maxillary incisors with the highest prevalence at 11-15 years of age [19]. It is also important to note that anterior maxillary over-jet protrusion malocclusion was a significant risk factor for the occurrence of traumatic dental injuries where children with a 6mm or more over-jet had a 4 times higher risk of suffering dental trauma compared to those with less or no over-jet [11].
The traumatic dental injuries that occur in children and adolescents are of two types, luxations and fractures. In a study of 4754 patients with 10,166 injured teeth it was found that 73.4% of the injured teeth sustained luxation type injuries and 58.2% sustained fracture type injuries. However, one third of all injured teeth in this study sustained a combination of both a fracture and luxation type injury, making luxation type injuries the most frequent occurrence [20].
The dental pulps of traumatically injured teeth may remain vital or may undergo necrosis or calcification depending upon the severity and type of injury, and the stage of tooth development [21-27]. The pulps of teeth that have sustained mild to moderate luxation injuries (concussion and subluxation) have a good chance of remaining vital [21,25-27], whereas the pulps of teeth that have sustained more severe luxation injuries (extrusive, intrusive and lateral luxation) have a poor prognosis for survival and will invariably undergo necrosis and require endodontic treatment [28-30]. It should be noted however, that for luxated teeth, pulp necrosis was significantly related to the dimension of the apical foramen, where a much higher incidence of pulp necrosis occurred in mature teeth with smaller apical foramen, and a lower rate of pulp necrosis occurred in immature teeth with larger apical foramen [31]. Additionally, the development of pulpal necrosis and periapicalpathosis may even occur well after the occurrence of mild traumatic injuries [21,22,24,26,27], therefore it is advisable to conduct periodic follow-up examinations for all traumatized teeth to determine their pulpal status and render endodontic treatment when indicated. Generally however, for fully developed and apically closed mature teeth that have sustained severe traumatic injuries, endodontic treatment should be initiated and should not be delayed beyond 2 weeks since the prognosis for pulp survival is very low and pulp necrosis is inevitable [21,22,28-30].
Contemporary treatment guidelines for the management of luxated permanent teeth, which are based on the type and severity of the injury and the stage of tooth development at the time of injury, recommend early pulp removal for severely luxated mature teeth where the possibility of pulp survival is very low and the probability of pulp necrosis is very high [32,33].
The purpose of this report was to present two clinical cases in which endodontic treatment of traumatically injured anterior permanent teeth, during active orthodontic treatment, for teenage orthodontic patients resulted in a favorable endodontic treatment outcome and promoted the normal progression of their orthodontic treatment.
Case 1
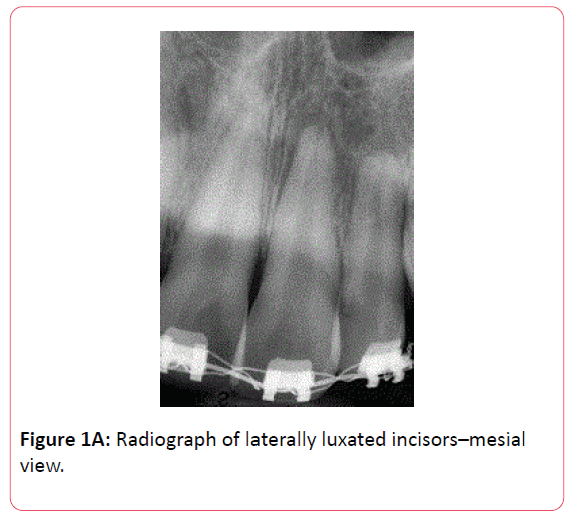
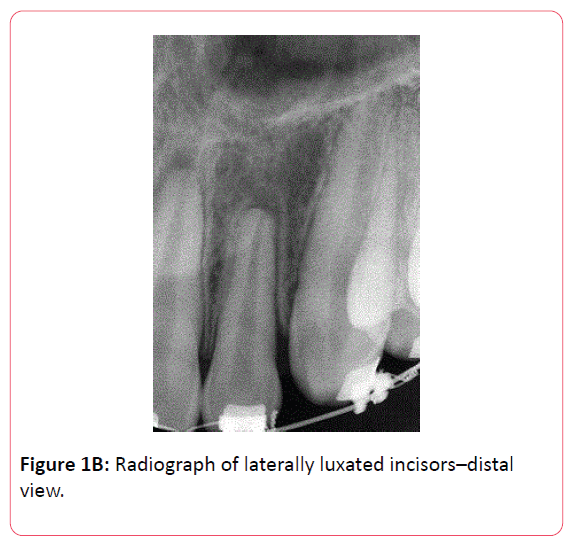
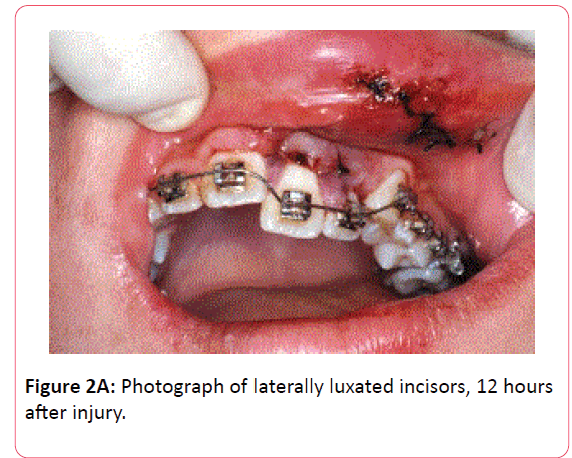
A 15 year old male, in good general health under active orthodontic treatment, presented with his parents to a hospital emergency room in the evening approximately 1 hour after he fell off his bicycle and his mouth and front teeth hit the bicycle handle bars. His vital signs were within normal limits and there were no apparent signs of head injuries or symptoms of concussion. His maxillary left central and lateral incisors were severely laterally luxated in a palatal direction and held in palatal displacement by the distorted orthodontic appliance. There was a vestibular laceration of the upper left lip and a labial laceration on the attached gingivae of the luxated left incisors which were cleaned and closed with 4/0 silk sutures. Ibuprofen 200 mg prn pain and Amoxicillin 500 mg q8h had been prescribed. Approximately 12 hours later the patient reported to the dental clinic for conjoint orthodontic and endodontic evaluation and radiographs were taken which showed the displacement of the maxillary left incisors with no root or alveolar bone fractures (Figures 1A and 1B).
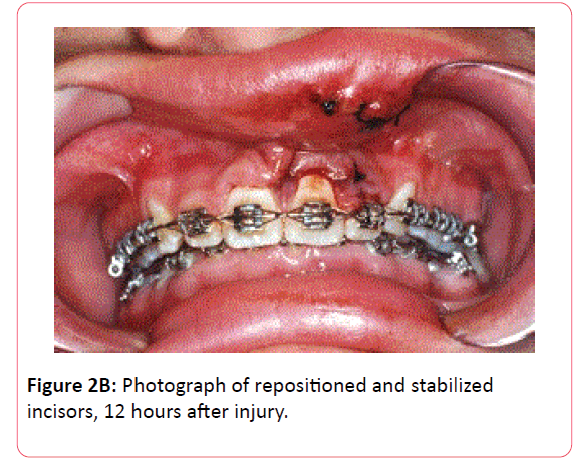
Clinical examination of the patient revealed the severely luxated incisors and gross distortion of the maxillary orthodontic arch wire (Figure 2A). Local anesthesia was administered by infiltration of 2 cartridges of 2% lidocaine with 1:100,000 epinephrine. The luxated incisors were digitally repositioned and realigned into normal position within their alveolar sockets and the maxillary arch wire was readjusted and reinforced to provide adequate stabilization of the anterior teeth (Figure 2B).
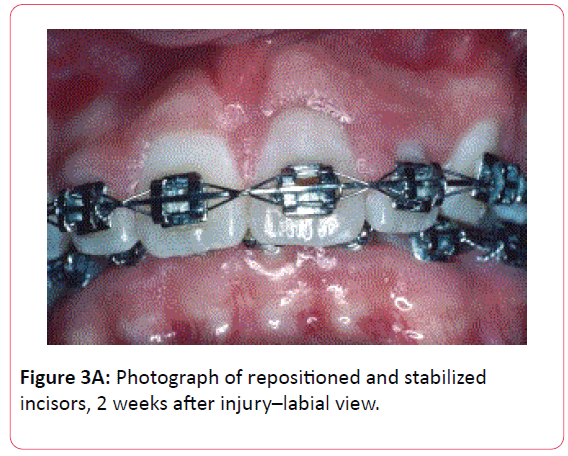
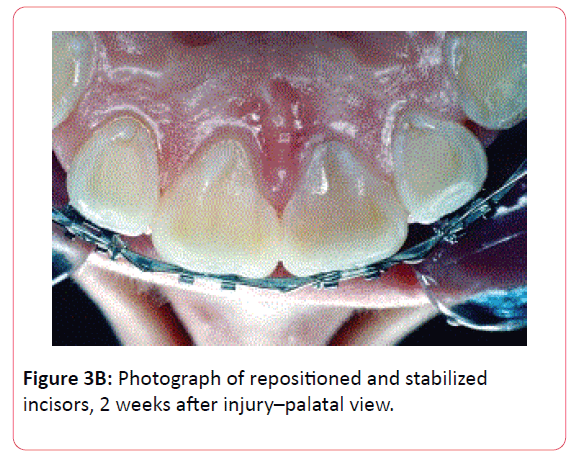
Two weeks later, clinical examination revealed that the lacerations had healed with loss of the sutures, the gingival and periodontal tissues of the repositioned and orthodontically stabilized maxillary left central and lateral incisors were healing normally, and the traumatized teeth were discolored and mildly sensitivity to percussion (Figures 3A and 3B).
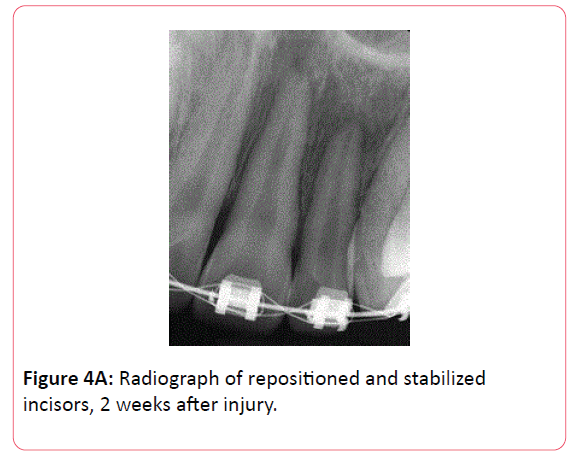
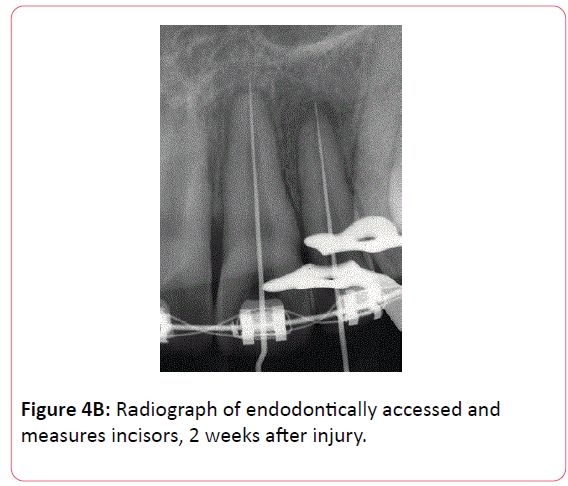
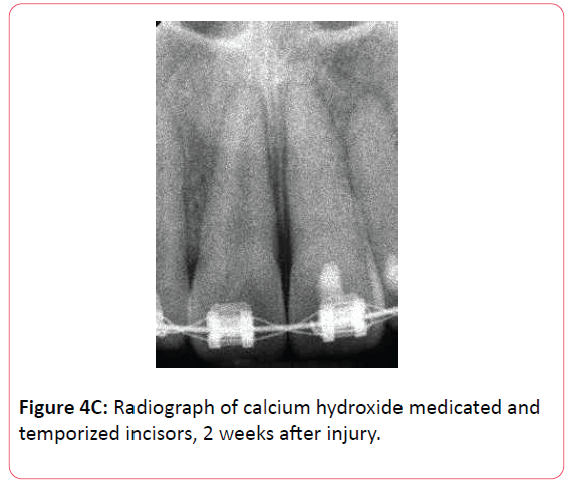
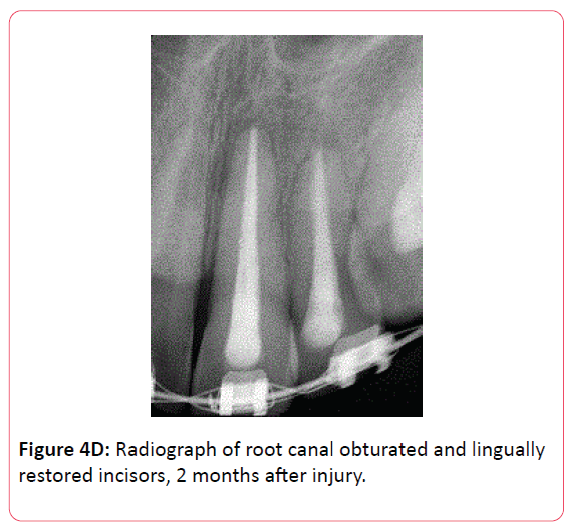
The maxillary right central and lateral incisors which probably had sustained concussion injuries pulp tested vital, while the luxated maxillary left incisors pulp tested nonvital. Radiographic examination showed that the bracketed and ligated maxillary left incisors were in good alignment and revealed mild periapical rarefactions due to their traumatic luxation (Figure 4A). The pulps of the maxillary right incisors were diagnosed as normal and the pulps of the maxillary left incisors were diagnosed as necrotic. Local anesthesia was administered by infiltration of 2 cartridges of 2% lidocaine with 1:100,000 epinephrine and the maxillary left central and lateral incisors were dental dam isolated, endodontically accessed and measured (Figure 4B), pulp extirpated, instrumented, irrigated, filled with a paste of calcium hydroxide USP and physiological saline, and temporized (Figure 4C). Six weeks later at 2 months after injury, with the patient comfortable and the traumatized incisors asymptomatic, the root canals of the left maxillary incisors were obturated with guttapercha and a calcium hydroxide based root canal sealer followed by lingual composite resin restorations (Figure 4D).
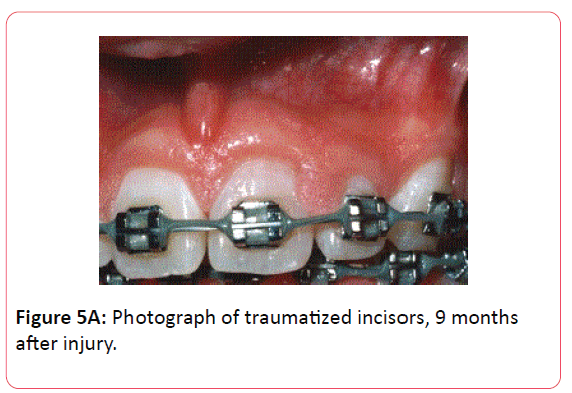
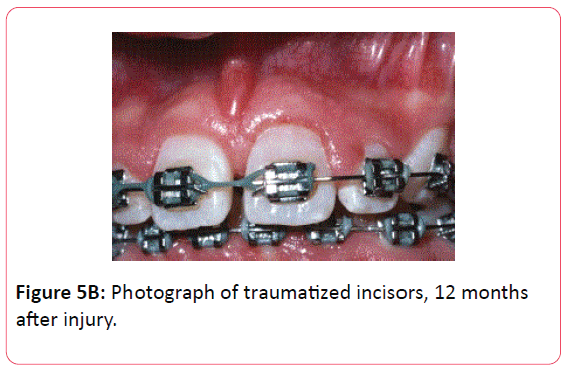
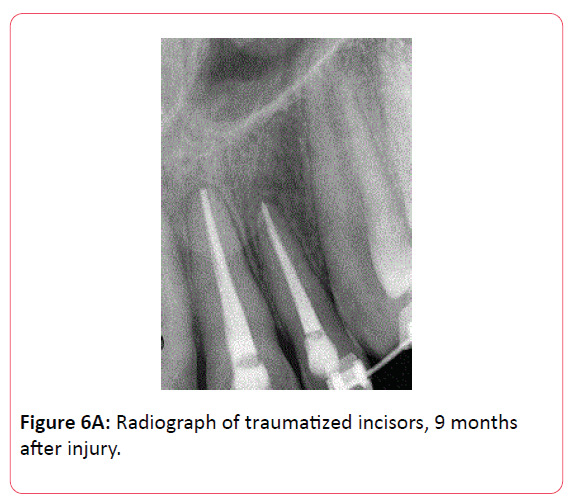
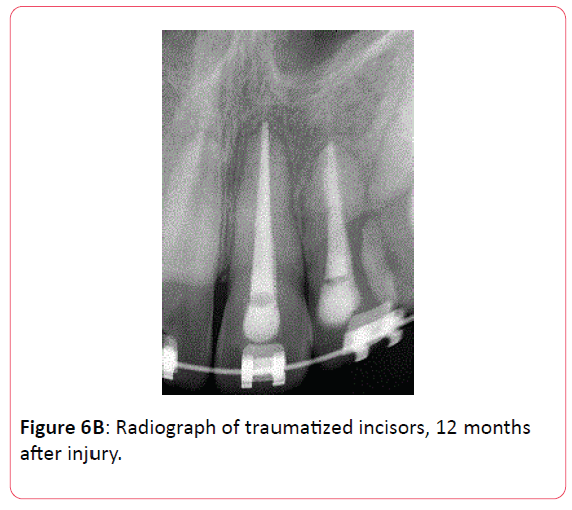
At 9 and 12 months recall all clinical examination parameters for the maxillary incisors were normal with good progression of the patient’s orthodontic treatment (Figures 5A and 5B). On radiographic examination of the maxillary left incisors, at 9 and 12 months recall, there were mild degrees of apical root resorption as sequelae of the traumatic luxations, however the periapical and periradicular radiographic appearances for both incisors were normal (Figures 6A and 6B).
Case 2
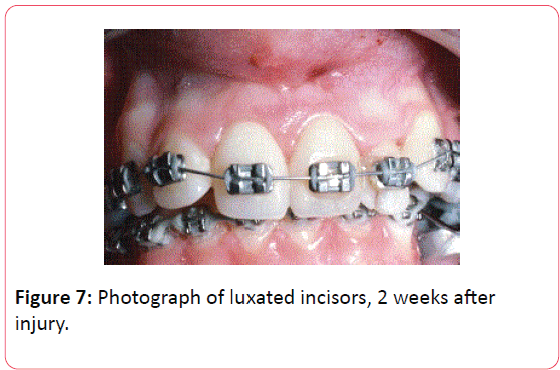
A 17 year old female, under orthodontic treatment for the past 3 years, reported to a hospital dental clinic approximately 2 hours after being accidentally hit in the face that resulted in the lateral luxation of her orthodontically bracket bonded and arch wired maxillary right and left central incisors and left lateral incisor. She was in good general health with a noncontributory medical history and her vital signs were within normal limits. Her orthodontic appliance had been distorted as a result of the displacement of the traumatized incisors which were firmly stable with no mobility. Her upper lip had sustained abrasions and contusions. Panoramic radiographic examination had revealed no apparent fractures of the teeth, alveolar bone or jaws. No attempt had been made to reposition the luxated teeth at the time of the accident. The lip abrasions had been cleaned, the contusions managed with ice-packs, and pain was controlled with Percocet (5 mg oxycodone and 500 mg acetaminophen) 1 q6h prn for 2 days. Conjoint orthodontic and endodontic assessment 2 weeks later, determined that since the repositioning of the luxated teeth had already been delayed, they would be orthodontically repositioned after endodontic evaluation and treatment. On clinical examination the patient was comfortable and the bracketed and wired luxated teeth were stable (Figure 7), however they were sensitive to percussion and tender to palpation, and pulp testing of the central incisors indicated non-vitality.
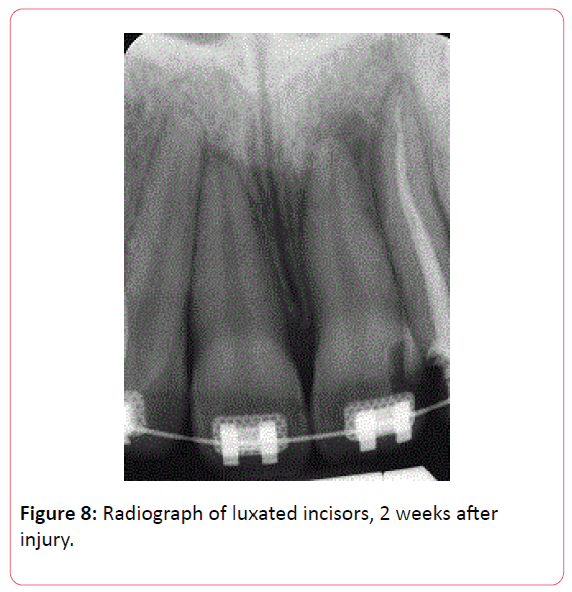
A diagnosis of pulpal necrosis with symptomatic apical periodontitis was made for both incisors. The lip abrasions and contusion had resolved and the gingival attachments around the luxated teeth were intact. The left central and lateral incisors had previously been restored with composite resins. Radiographic examination revealed that the left lateral incisor had prior root canal treatment and all three luxated incisors exhibited mild periapical rarefactions caused by the traumatic luxation injuries (Figure 8).
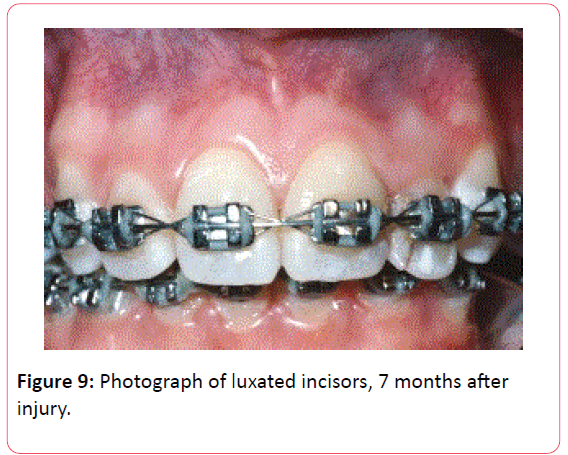
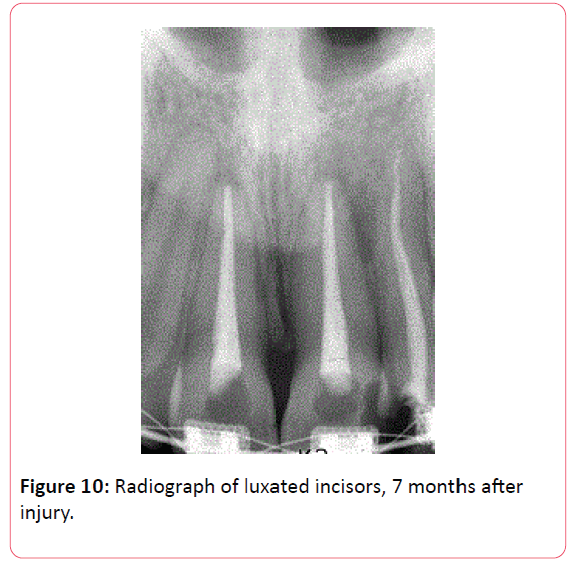
Local anesthesia was administered by infiltration of 2 cartridges of 2% lidocaine with 1:100,000 epinephrine. The maxillary central incisors were dental dam isolated, endodontically accessed, measured, pulp extirpated, instrumented, irrigated, filled with a paste of calcium hydroxide USP and physiological saline, and the access cavities temporized. The maxillary left lateral incisor was not endodontically retreated. One month later with the patient comfortable and the teeth asymptomatic, the root canals of the central incisors were obturated with guttapercha and a calcium hydroxide based root canal sealer followed by lingual composite resin restorations. Repositioning of the luxated incisors then commenced with the resumption of orthodontic treatment. At recall examination 7 months after injury, clinical examination reveled that the luxated incisors were in good realignment with intact gingival attachments, normal periodontium and good progression of orthodontic treatment (Figure 9). Radiograph examination of the luxated teeth showed slight apical root resorption and normal appearing periapices (Figure 10).
Discussion
The assessment process for traumatic dental injuries in orthodontic patients should be based on an accurate account of the traumatic event, and a clinical maxillofacial and dentoalveolar examination to determine the presence of soft tissue injuries and swelling, tenderness to palpation, bony crepitus, tooth dislocation and mobility, crown discoloration or fracture, reactions of the teeth to percussion and responses of the pulp to testing, and an evaluation of angulated periapical radiographs for the presence of root or alveolar bone fractures [34]. The clinician should take into consideration the age and dental development of the patient and the type and severity of the dental injuries sustained, with particular attention given to the degree of tooth mobility and the extent and direction of tooth displacement, since these conditions impact on the survival of the pulp and the healing of the periodontal tissues [35]. This was the protocol followed in the examination and diagnosis of the traumatic dental injuries that occurred during the active orthodontic treatment of the teenage patients in the case reports presented, and was consistent with that described by Kindelan et al., and Day et al. in their overview accounts of the influence of dental trauma in the management orthodontic treatment [34,35].
Patients who have sustained severe luxation injuries to mature maxillary permanent incisors with fully closes apices, will invariably require endodontic treatment, which should be initiated soon after the injury to avoid apical periodontitis and inflammatory root resorption due to pulpal necrosis [21,22,26]. Pulp extirpation and placement of a calcium hydroxide intra-root-canal dressing in the severely luxated maxillary permanent incisors for theadolescent orthodontic patients in the cases here presented was accomplished at 2 weeks after injury, in accordance with the treatment guidelines for the management of severely luxated teeth [32,33], and root canal obturation with guttapercha and root canal sealer followed shortly thereafter.
In both Cases 1 and 2, periapical rarefactions associated with the luxated anterior incisors were radiographically observed 2 weeks after traumatic injury. The occurrence of periapical rarefactions that initially appear after traumatic luxations and then later resolve has been reported and described as a transient apical breakdown [36]. However, when severe luxation injuries occur to fully developed mature permanent teeth, periapical inflammatory reactions with the development of periapical rarefactions are signs associated with pulpal ischemia as a result of disruption of the apical vasculature with impending pulpal necrosis [22,26,27]. Ischemic injury to the dental pulp can even occur with mild luxation injuries, that may eventually lead to pulpal necrosis or pulpal calcification, well after the trauma [23,24,27]. In the cases here presented of adolescent orthodontic patients who sustained severe luxation injuries to their maxillary permanent incisors during active orthodontic treatment, endodontic management was promptly initiated and completed in a timely manner, in agreement with the guidelines of the International Association of Dental Traumatology [32,33], which allowed for the continuation of their orthodontic treatment.
Traumatically disarticulated teeth are generally repositioned and splint stabilized at the time of the injury [32,33]. In Case 1, the traumatically luxated incisors had not been immediately repositioned after injury, but were able to be repositioned 12 hours after injury while they were still movable and had not undergone periodontal reattachment. In Case 2, two weeks had already passed after the injury and the traumatically luxated incisors were immobile and stable in their displaced position having undergone some degree of periodontal reattachment. Forceful repositioning at that time would have caused additional injury to the partially reattached periodontal tissues, resulting in further complications. Therefore, physiologic orthodontic tooth movement was considered to be the method of choice and was followed for repositioning these teeth. It is important for the clinician, in managing traumatic injuries in orthodontic patients, to tailor the treatment to the particular clinical conditions that are presented by the patient.
The outcome criteria for success of endodontically treated traumatized anterior permanent teeth, determined at an appropriate follow-up recall examination, should follow a standard assessment protocol [37]. This includes visual inspection of the intra-oral soft tissues for evidence of swelling or sinus tract stomas, palpation of the alveolar mucosa for signs of tissue tenderness, and percussion of the teeth for signs of pain [37]. The endodontically treated traumatized teeth should be asymptomatic and functioning, have intact gingival attachments, normal mobility, and no indications of tooth ankylosis [37]. Also, the recall radiographs should verify the absence of periapical or periradicularradiolucencies and the presence of normal alveolar bone [37]. These were the outcome criteria used for assessment of the endodontic treatment in the cases here presented, which were successfully achieved, in accordance with the quality assurance guidelines of the European Society of Endodontics [37].
There were however, mild apical root resorptions observed on follow-up examinations for the traumatized maxillary incisors in both Case 1 and 2. Apical root resorption can result from orthodontic tooth movement [34,35,38,39], and traumatized teeth may be at an increased risk for further apical root resorption as a result of orthodontic tooth movement forces [34,35,40,41]. Therefore, the findings of mild apical root resorptions for the traumatized maxillary permanent incisors in the cases presented were not unusual.
Teenage orthodontic patients who sustain dental trauma during active orthodontic treatment will inevitability require endodontic treatment to support the progress and prognosis of their orthodontic treatment. Communication and cooperation between the orthodontist and endodontist is essential and cannot be overemphasized for the management of traumatic dental injuries in adolescent orthodontic patients. A professionally integrated clinical management approach was followed in the cases here presented, in agreement with authors who have addressed the benefits of interdisciplinary patient care [34,35,42].
Acknowledgement
The author has no conflicts of interests.
Conclusions
1. Successful endodontic treatment results and resumption of orthodontic treatment were achieved for teenage orthodontic patients who sustained traumatic dental injuries to their maxillary permanent incisors during active orthodontic treatment.
2. An interdisciplinary patient management approach was beneficial in achieving favourable endodontic and orthodontic treatment outcomes for teenage orthodontic patients who sustained traumatic dental injuries during active orthodontic treatment.
References
- United States Department of Health and Human Services, National Centre for Health Statistics, National Health and Nutrition Examination Surveys, (NHANES I) 1971-1974, (NHANES II) 1976-1980, and (NHANES III) 1988-1994 Washington DC, USA.
- Kelley JE, Sanchez M, Van Kirk LE (1973) An assessment of the occlusion of the teeth of children 6-11 years. DHEW Publication, National Centre for Health Statistics, Washington, DC.
- Christopherson EA, Briskie D, Inglehart MR (2009) Objective, subjective, and self-assessment of preadolescent orthodontic treatment need: a function of age, gender, and ethnic/racial background. J Public Health Dent 69: 9-17.
- Christopherson EA, Briskie D, Inglehart MR (2009) Preadolescent orthodontic treatment need: objective and subjective provider assessments and patient self-reports. Am J Orthod Dentofacial Orthop 135: 80-86.
- Proffit WR, Fields HW, Moray L (1998) Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg 12: 97-106.
- Gabris K, Tarjan I, Rozsa N (2001) Dental trauma in children presenting for treatment at the Department of Dentistry for Children and Orthodontics, Budapest, 1985 – 1999. Dental Traimatol 17: 103-108.
- Al-Mejad I, Murry JJ, Maguire A (2001) The prevalence of dental trauma in 5-6 and 12-14 year old boys in Riyadh, Saudi Arabia. Dent Traumatol 17: 153-158.
- Al-Jundi SH (2001) Dental emergencies presenting to a dental teaching hospital due tocomplications from traumatic dental injuries. Dent Traumatol 18: 181-185.
- Wright G, Bell A, McGlashan G, Vincent C, Wellbury RR (2007) Dentoalveolar trauma in Glasgow: an audit of mechanism and injury. Dent Traumatol 23:226-231.
- Diaz JA, Bustos L, Brandt AC, Fernandez BE (2010) Dental injuries among children and adolescents aged 1–15 years attending to public hospital in Temuco, Chile. Dent Traumatol 26: 254-261.
- Schatz JP, Hakeberg M, Ostine E, Killaridis S (2013) Prevalence of traumatic injuries to the permanent dentition and its association with overjet in a Swiss child population. Dent Traumatol 29:110-114.
- Ankola AV, Hebbal M, Sharma S, Nayak SS (2013) Traumatic dental injuries in primary school children of South India – a report from district-wide oral health survey. Dent Traumatol 29: 134-138.
- Oldin A, Lundgren J, Nilsson M, Noren JG, Robertson A (2015) Traumatic dental injuries among children aged 0-17 years in the BITA study – A longitudinal Swedish multicenter study. Dent Traumatol 31: 9-17.
- Bilder L, Margvelashvill V, Sgan-Cohen H, Kalandadze M, Levin L, et al. (2015) Traumatic dental injuries among 12 and 15 year old adolescents in Georgia: results of the pathfinder study. Dent Traumatol 31: 1-5.
- Glendor U (2008) Epidemiology of traumatic dental injuries – a 12 year review of theliterature. Dent Traumatol 24: 603-611.
- Glendor U (2009) Aetiology and risk factors related to traumatic dental injuries – a review of the litetature. Dent Traumatol 25:19-31.
- Skaare AB, Jacobsen I (2003) Dental injuries in Norwegians aged 7-18 years. Dent Traumatol 19: 67-71.
- Loxomboon D, Carison C, Andersson R, von Bultzingslowen I, Mensah T (2016) Incidence and cases of dental trauma in children living in the county of Varmland, Sweden.Dent Traumatol 32: 58-64.
- Bauss O, Rohlong J, Schwestka-Polly R (2004) Prevalence of traumatic injuries to the permanent incisors in candidates for orthodontic treatment. Dent Traumatol 20: 61-66.
- Lauridsen E, Hermann NV, Gerds TA, Krelborg S, Andreasen JO (2012) Pattern of traumatic dental injuries in the permanent dentition among children, adolescents, and adults. Dent Traumatol 28: 358-363.
- Andreasen JO (1970) Luxation of permanent teeth due to trauma: A clinical and radiographic follow-up study of 189 injured teeth. Scand J Dent Res 78: 273-286.
- Andreasen FM, Vestergaard Pedersen B (1985) Prognosis of luxated permanent teeth – the development of pulp necrosis. Endod Dent Traumatol 1: 207-220.
- Andreasen FM, Yu Z, Thombsen B, Andersen PK (1987) Occurrence of pulp canal obliteration after luxation injuries in the permanent dentition. Endod Dent Traumatol 3: 103-105.
- Oikarinen K, Gundlach KKH, Pfeifer G (1987) Late complications of luxation injuries to teeth. Endod Dent Traumatol 3: 296-303.
- Andreasen FM (1989) Pulpal healing after luxation injuries and root fracture in the permanent dentition. Endod Dent Traumatol 5: 111-131.
- Crona-Larsson G, Bjarnason S, Noren JG (1991) Effects of luxation injuries on permanent teeth. Endod Dent Traumatol 7: 199-206.
- Feiglin B (1996) Dental pulp response to traumatic injuries – a retrospective analysis with case reports. Endod Dent Traumatol 12: 1-8.
- Humphrey JM, Kenny DJ, Barret EJ (2003) Clinical outcomes for permanent incisorluxations in a pediatric population. I. Intrusions. Dent Traumatol 19: 266-273.
- Lee R, Barret EJ, Kenny DJ (2003) Clinical outcomes for permanent incisor luxationsin a pediatric population. II. Extrusions. Dent Traumatol 19: 274-279.
- Nikoui M, Kenny DJ, Barret EJ (2003) Clinical outcomes for permanent incisor luxations a pediatric population. III. Lateral luxations. Dent Traumatol 19: 280-285.
- Andreasen FM, Zhijie Y, Thomsen B (1986) Relationship between pulp dimensions and development of pulp necrosis after luxation injuries in the permanent dentition. Endod Dent Traumatol 2: 90-98.
- Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, et al. (2007) Guidelines for the management of traumatic dental injuries. I Fractures and luxations of permanent teeth. Dent Traumatol 23: 66-71.
- DiAngelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, et al. (2012) International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol pp: 2-12.
- Kindelan SA, Day PF, Kindelen JD, Spencer JR, Duggal MS (2008) Dental trauma: An overview of its influence on the management of orthodontic treatment. Part 1. J Orthod 35: 68-78.
- Day PF, Kindelan SA, Spencer JR, Kindelen JD, Duggal MS (2008). Dental trauma:Part 2. Managing poor prognosis anterior teeth – treatment options for the subsequent space in a growing patient. J Orthod 35:143-155.
- Andreasen FM (1986) Transient apical breakdown and its relation to color and sensibility changes after lxation injuries to teeth. Endod Dent Traumatol 2: 9-19.
- European Society of Endodontics (1994) Consensus report on quality guidelines for endodontic treatment. Int Endod J 27: 115-124.
- Levander E, Malmgren O (1988) Evaluation of the risk of root resorption during orthodontic treatment: A study of upper incisors. Eur J Orthod 10: 30-38.
- Levander E, Bajka R, Malmgren O (1998) Early radiographic diagnosis of apical root resorption during orthodontic treatment: a study of maxillary incisors. Eur J Orthod 20: 57-63.
- Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, et al. (1982) Root resorptionafter orthodontic treatment of traumatized teeth. Am J Orthod 82: 487-491.
- Linge BO, Linge L (1983) Apical root resorption in upper anterior teeth. Eur J Orthod 5: 173-183.
- Hamilton RS, Gutmann JL (1999) Endodontic-orthodontic relationships: a review of integrated treatment planning. Int Endod J 32: 343-360.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences