Interdisciplinary Approach Using Mini-Implants Anchorage ÃÆâÃâââ¬Ãâââ¬Å A Case Report
Luciana Aparecida Sousa Iwamoto, Gerson Yoshinobu Iwamoto, Monica Talarico Duailibi, Rosa Carriere Rossi, Silvio Eduardo Duailibi
Luciana Aparecida Sousa Iwamoto*, Gerson Yoshinobu Iwamoto, Monica Talarico Duailibi, Rosa Carriere Rossi, Silvio Eduardo Duailibi
Universidade Federal de Sao Paulo
- *Corresponding Author:
- Luciana Aparecida Sousa Iwamoto
Universidade Federal de Sao Paulo
São Paulo, Brazil
Tel: 55 11 22044550
E-mail: lasiwamoto@hotmail.com
Abstract
Implants and mini-implants have been used in orthodontics as an important method of anchorage. This method allows the treatment with minimal patients? cooperation, and also serves as a support for various types of orthodontic movement. The anchorage control is fundamental to the success of orthodontic treatment because of its rigid fixation in the bone. Mini-implants are easily installed, especially using computerized surgical guides. As an additional advantage, they enable the use of various accessories. This paper aims to describe the steps of a detailed preoperative planning for mini-implants through a case study report in order to improve treatment success. Specific software was used for planning and production of a surgical guide with a highly accurate and minimally invasive protocol, through CT and prototypes, increasing accuracy and assertiveness procedures. The success of the treatment was achieved, and the miniimplant remained in function throughout the active orthodontic treatment. Merging technology with technical knowledge leads the modern dentistry excellence in several areas as diagnosis, planning and prototyping. However, before installing the mini-implants, it is necessary previous knowledge of the desired movements, understanding the bone?s quality and quantity, biomechanics installation and orthodontic movements.
Keywords
Computer assisted surgery; Orthodontics Anchorage; Dental implants
Introduction
The integration of different dental specialties, for example orthodontics and implantology, has been growing lately. Orthodontics collaborates on oral rehabilitation cases by correcting the wrong dental positioning, facilitating and enabling the installation of implants and prostheses. Similarly, implants can be added to improve orthodontic dental movements.
Obtaining anchor points is one of the critical features of orthodontic treatment. Anchorage is defined as a resistance movement, which follows the principle of Newton’s Third Law of motion (action and reaction). In this case, the reaction to the applied force is orthodontic tooth movement [1]. The use of adjacent teeth is the most common method used to obtain anchorage. However, it can cause collateral effects on support teeth and can provide a no adequate anchorage. Therefore, orthodontics uses extra-oral anchorage as leverage points at cervical, cranial and facial regions. The use of extra-oral devices requires the patients’ cooperation, interferes on the aesthetic, and also can also present functional complications [2].
Upon seeking a solution for this problem, Gainsforth & Higley (1945), suggested the use of anchorage through intra-oral implants [3-5].
The use of implants for orthodontic anchorage began when orthodontics started using prosthetic rehabilitation with implants performed as anchor points for moving teeth. More recently, mini-implants have been developed for specific orthodontic anchorage, they can be installed strategically in order to provide the best possible anchorage. Currently implants and miniimplants are important devices for anchorage methods, enabling or facilitating complex orthodontic movements, such as anterior retraction, intrusion, extrusion, distal, mesial and vertical movements [1].
Mini-implants, whose dimensions may range from 1.2 to 2 mm in diameter, and 6 to 12mm in length, may be made of titanium or stainless steel. These implants can have various orthodontic accessories attached (brackets and buttons of various sizes and shapes), in order to make easier the installation of orthodontic tie wire and elastic moduli. According Deguchi et al. (2003), the miniimplants have advantages over the regular implants because of their small size, enabling the installation of a larger number of sites in the mouth, causing less surgical trauma, and could reduce and/or eliminate preload during the healing period.
The interrelationship between orthodontics and implantology offers to professionals, possible solutions to solve diverse clinical situations, and can improve the oral rehabilitation according Di Mateo & Sendik (2005).
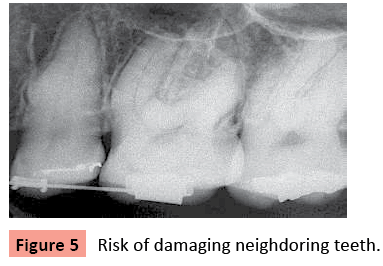
With the advent of computerized surgical guide, the risk of damage to adjacent structures decreased, thus allowing greater safety in the installation of mini-implants [6,7] .
Objective
This paper aims to describe the steps of a detailed preoperative planning for mini-implants used in a succeeded case of orthodontic treatment, helping on improvement of success in similar cases. Treatment planning was designed by specific software through CT and model; the results were transported by prototyped guides, increasing accuracy and assertiveness procedures, seeking the diagnosis, planning and accurate guide.
Case
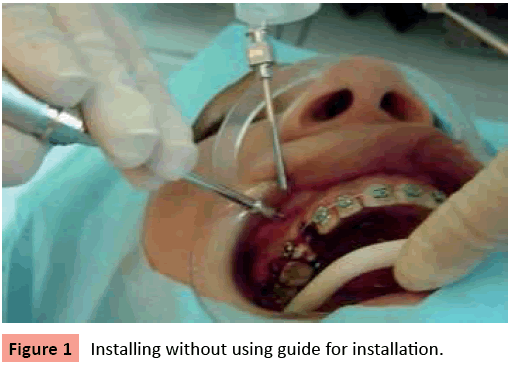
A patient female, JPS, 22 years old, underwent surgical procedures so that anchorage through implants could be set up (Figure1,2). At the planning phase it was decided to use the self-threaded mini-implant with immediate load.
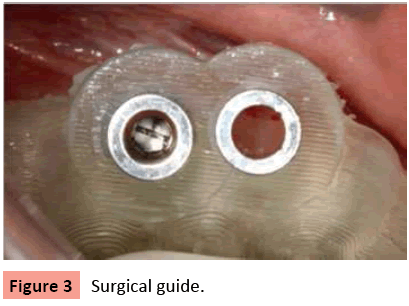
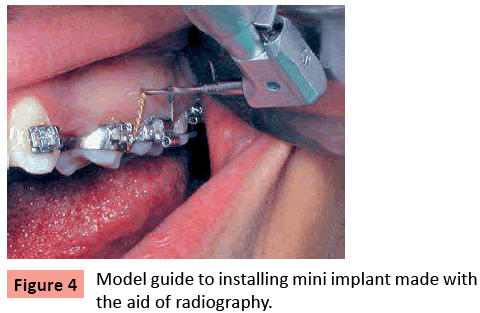
Surgical protocol: Cone-bean computed tomography was performed, and the obtained images were transferred to the software and to the study model, producing an accurate surgical guide with 3D technology [6], (Figure 3).
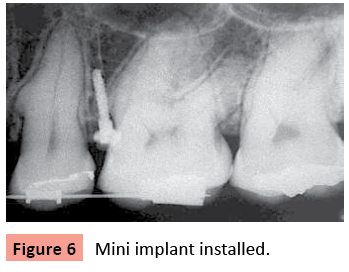
The surgical technique for installation of orthodontic miniimplants followed a strict accomplishment protocol, with the addition of a surgical guide to avoid injuries, especially in adjacent roots, during fixation [1,8] (Figure 3, 4). The surgery was performed at a dental office; local infiltration anesthesia with subperiosteal Citanest 3% was applied in order to allow the patient’s perception of any possible unwanted contact at neighboring anatomical structures. The osteotomy was performed by motor for implant rotation in 1500 RPM and reduced at 1/16, under saline irrigation to avoid heating the bone, and using twist drill smaller than the mini implant to be installed, thus providing better implant stability by the exact fixation of its surface to the bone wall. Osteotomy can also be done by itself when miniimplants are self-threaded, increasing bone primary stability. The mini-implant must be installed under irrigation, using a manual tool or a low-speed surgical motor. The surgical time, considering the drilling and insertion of mini-implant trans-mucosal, does not usually take more than five minutes. However, the total procedure time including assetpia, anesthesia, adaptation of the guide, mini-implant installation and peri-implant hygiene orientation takes approximately thirty minutes.
The case report demonstrates the need for a careful of installating mini-implants (Figure 5),(Figure 6).All guides are efficient; however, computerized tomography greatly reduces the risk of reaching the neighboring teeth roots [6-32].
Discussion
Before the procedures, a careful planning must be done, including the choice of location, type, size, and the level of force applied on the mini-implant. Traumatic surgery can be avoided by the use of low-speed motor, and adequate irrigation to prevent bone heating during drilling. Also, avoiding I=installation of mini-implants in alveolar mucosa. When possible, it is recommended using thicker implants or two implants conjugated in patients with thin cortical. No excessive force should be applied on the miniimplant during treatment, including pressure caused by patients’ tongue or finger. Moreover, providing guidance to patients about oral hygiene around the implant in order to prevent inflammation will improve the treatment success rate.
Merging technology with the technical knowledge leads modern dentistry to obtain excellence in the areas of diagnosis, planning and prototyping. Further research should be carried to standardize the use of implant-orthodontic. Although the results are satisfactory, the systematization presents easier interventions, and, from the legal point of view, it will encourage and provide security to biomechanical solutions. Finally, the patients’ psychological aspect must be worked out when this type of intervention is indicated.
References
- Laboissere Jr., M., Villele H., Bezerra F., Laboissere M., Diaz L. (2005) Ancoragem absoluta utilizando microparafusos ortodônticos: complicações e fatores de risco ( Trilogia- Pt III). ImplantNews. 2: 165-168.
- Padovan L.E.M, Thomé G, Melo A.C.M, Assis D.S.F.R., Souza, P.C.U (2006) Utilização de microimplantes como ancoragem ortodôntica no tratamento das más-oclusões. Implant News. 3: 163-166.
- Gainsforth, B.L., Higley, L.B.(1945) A study of orthodontic anchorage possibilities in basal bone. Am J Orthod Oral Surg. 31:406-416.
- Deguchi T, Takano-Yamamoto T, Kanomi R, Hartsfield JK Jr, Roberts WE, et al. (2003) The use of small titanium screws for orthodontic anchorage.J Dent Res 82: 377-381.
- Di Mateo, R.C., Villa, N., Sendyk, W.R. (2005) Movimentação de molares inferiores ancorados em miniparafusos.R Dental Press ORthodon Ortop Facial. 10:124-133
- Yu J.J, Kim G.T, Choi Y.S, Hwang E.H, Paek J et.al (2012) Accuracy of a cone beam computed tomography-guided surgical stent for orthodontic mini-implant placement. Angle Orthod. 82:275-283.
- Kim SH, Cho JH, Chung KR, Kook YA, Nelson G (2008) Removal torque values of surface-treated mini-implants after loading.Am J Orthod Dentofacial Orthop 134: 36-43.
- DE Vico G, Spinelli D, Bonino M, Schiavetti R, Pozzi A, et al. (2012) Computer-assisted virtual treatment planning combined with flapless surgery and immediate loading in the rehabilitation of partial edentulies.Oral Implantol (Rome) 5: 3-10.
- Marassi C., Leal A., Herdy J.L., Chianelli O., Sobreira D. O. (2005) Uso de mini-implantes como auxiliares do tratamento ortodôntico. SPO. 38:256-265
- Akin-Nergiz N, Nergiz I, Schulz A, Arpak N, Niedermeier W (1998) Reactions of peri-implant tissues to continuous loading of osseointegrated implants.Am J Orthod Dentofacial Orthop 114: 292-298.
- Daimaruya T, Takahashi I, Nagasaka H, Umemori M, Sugawara J, et al. (2003) Effects of maxillary molar intrusion on the nasal floor and tooth root using the skeletal anchorage system in dogs.Angle Orthod 73: 158-166.
- Liou EJ, Pai BC, Lin JC (2004) Do miniscrews remain stationary under orthodontic forces?Am J Orthod Dentofacial Orthop 126: 42-47.
- Park, H.S. (2002) An anatomical study using CT images for the implantation of micro-implants. Kora J Orthod. 32: 435-441
- Park HS, Kwon TG, Sung JH (2004) Nonextraction treatment with microscrew implants.Angle Orthod 74: 539-549.
- Cheng SJ, Tseng IY, Lee JJ, Kok SH (2004) A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage.Int J Oral Maxillofac Implants 19: 100-106.
- Favero L, Brollo P, Bressan E (2002) Orthodontic anchorage with specific fixtures: related study analysis.Am J Orthod Dentofacial Orthop 122: 84-94.
- Bezzerra F., Vilella H., Laboissière Jr M., Diaz L.(2004) Ancoragem absoluta utilizando microparafusos ortodônticos de titânio. Planejamento e protocolo cirúrgico. Implant news (Trilogia –Parte I). 1: 469- 475.
- Kyung HM, Park HS, Bae SM, Sung JH, Kim IB (2003) Development of orthodontic micro-implants for intraoral anchorage.J Clin Orthod 37: 321-328.
- Rocha Filho, L. A. & Gadotti, R.J. (2008) Utilização de miniimplante como ancoragem ortodôntica. Implante News. 5:311-315.
- Aldikaçti M, Açikgöz G, Türk T, Trisi P (2004) Long-term evaluation of sandblasted and acid-etched implants used as orthodontic anchors in dogs.Am J Orthod Dentofacial Orthop 125: 139-147.
- Araújo, T.M., Nascimento, M. H. A., Bezerra, F., Sobral, M.C. (2006) Ancoragem esquelética em orthodontia com miniimplantes. R Dental Press Orthodon Ortop Facial.; v.11, n.4, p.126-56
- Deguchi T, Takano-Yamamoto T, Yabuuchi T, Ando R, Roberts WE, et al. (2008) Histomorphometric evaluation of alveolar bone turnover between the maxilla and the mandible during experimental tooth movement in dogs.Am J Orthod Dentofacial Orthop 133: 889-897.
- Daimaruya T, Nagasaka H, Umemori M, Sugawara J, Mitani H (2001) The influences of molar intrusion on the inferior alveolar neurovascular bundle and root using the skeletal anchorage system in dogs.Angle Orthod 71: 60-70.
- Fritz U, Diedrich P, Kinzinger G, Al-Said M (2003) The anchorage quality of mini-implants towards translatory and extrusive forces.J Orofac Orthop 64: 293-304.
- Janssen KI, Raghoebar GM, Vissink A, Sandham A (2008) Skeletal anchorage in orthodontics--a review of various systems in animal and human studies.Int J Oral Maxillofac Implants 23: 75-88.
- Huang LH, Shotwell JL, Wang HL (2005) Dental implants for orthodontic anchorage.Am J Orthod Dentofacial Orthop 127: 713-722.
- Kim S.H., Choi Y.S., Hwang E.H., Chung K.R., Kook Y.A., Nelson G. (2007) Surgical positioning of orthodontic mini-implants with guides fabricated on models replicated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop.131:S82-89.
- Lim JE, Lim WH, Chun YS (2008) Quantitative evaluation of cortical bone thickness and root proximity at maxillary interradicular sites for orthodontic mini-implant placement.Clin Anat 21: 486-491.
- Maino BG, Bednar J, Pagin P, Mura P (2003) The spider screw for skeletal anchorage.J Clin Orthod 37: 90-97.
- Männchen R, Schätzle M (2008) Success rate of palatal orthodontic implants: a prospective longitudinal study.Clin Oral Implants Res 19: 665-669.
- Nascimento M.H., Araujo T.M., Bezerra F (2006) Microparafuso ortodôntico: inatalação e orientação de higiene periimplantar. R Clin Ortodon Dental Press, Maringá, v. 5, n. 1 - fev./mar
- Oyonarte R, Pilliar RM, Deporter D, Woodside DG (2005) Peri-implant bone response to orthodontic loading: Part 2. Implant surface geometry and its effect on regional bone remodeling.Am J Orthod Dentofacial Orthop 128: 182-189.
- Suzuki EY, Suzuki B (2008) Accuracy of miniscrew implant placement with a 3-dimensional surgical guide.J Oral Maxillofac Surg 66: 1245-1252.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences