Latest in Research on Miniscrew Implants: An Interview with Ankit H Shah
Ankit H Shah
DOI10.21767/2469-2980.100024
Private practice, Dallas, TX, USA
- *Corresponding Author:
- Ankit H. Shah
Private practice, Dallas, TX, USA
E-mail: ankitshah.dds@gmail.com
Received date: March 16, 2016; Accepted date: April 07, 2016; Published date: April 11, 2016
Copyright: © 2016 Shah AH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Dr. Shah graduated from the world-renowned orthodontic residency program of Saint Louis University with a Master of Science (Research) degree and a Certificate in Orthodontics. Miniscrew implants are his primary area of research interest and he has published many scientific articles on this topic. He serves as a peer-reviewer for several high-impact orthodontic journals like the American Journal of Orthodontics & Dentofacial Orthopedics, the Angle Orthodontist and European Journal of Orthodontics.
Editor:
Please tell us about your research on the shorter miniscrew implants (MSIs).
Dr. Shah:
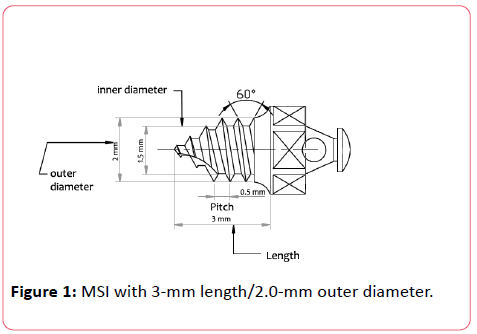
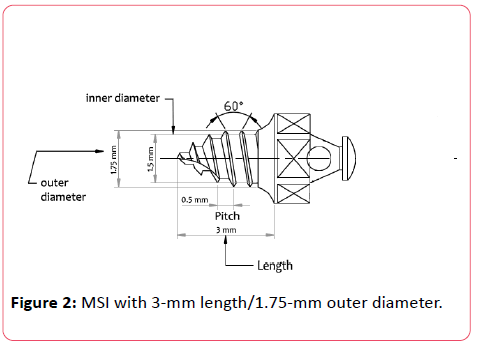
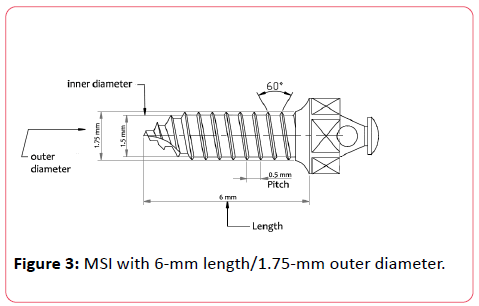
Anatomic limitations create a lot of drawbacks for the longer (6-mm and greater) MSIs. Since cortical plate is the main point of purchase for MSIs, I decided to investigate the feasibility of shorter (3-mm) MSIs for clinical application in orthodontics. I studied the effects of altering implant length, outer diameter, cortical bone thickness, and cortical bone density on the primary stability of shorter (3-mm) orthodontic MSIs. [1] Three MSI designs were evaluated: 3-mm length/2.0- mm outer diameter (Figure 1), 3-mm length/1.75-mm outer diameter (Figure 2) and 6-mm length/1.75-mm outer diameter (Figure 3).
The 3-mm MSIs showed less insertion torque and pullout strength than the 6-mm MSIs. However, the values were found to be above the limit that had been previously recommended for optimal stability. Insertion torque in my study was consistently greater than the 4 Ncm needed to provide optimal anchorage for MSIs. [2] Most importantly, the pullout forces of all the 3-mm MSIs, especially those 2-mm wide, were also considerably greater than the forces that are usually applied for tooth movements (30–400 grams) and orthopedic changes (500–1000 grams). [3, 4]
The overall findings of the above study are exciting! A small increase in the outer diameter of a 3-mm long MSI compensates for the reduction in its length significantly. This 3-mm long MSI provides us with a new alternative that can avoid damage to the teeth and surrounding structures due to its smaller length. From a clinical standpoint, these findings open up the vast possibility of use of shorter MSIs as an alternative to the longer MSIs typically used by orthodontists.
Editor:
What are the effects of altering implant length, outer diameter, cortical bone thickness, and cortical bone density on the primary stability of orthodontic MSIs?
Dr. Shah:
Several studies have shown that an increase in screw diameter can efficiently reinforce the initial stability of the MSIs. [5, 6] In fact, implant diameter is one of the most influential screw factors that can maximize the pullout strength. [7] MSI length is an equally important factor as maximum insertion torque of the MSI increases upon increasing the screw length, thereby having a positive impact on its primary stability. [5]
Increases in cortical bone thickness and cortical bone density also increase the primary stability of the MSIs. [8] Significant increase in insertion torque and pullout strength occurs when MSIs are inserted into areas with thicker cortical bone.
Greater amounts of bone (higher bone density) also increase the amount of bone-to-implant contact and greater engagement of bone by MSI threads, both of which contribute to increase in the pullout strength. [9]
Editor:
What are the advantages and disadvantages of MSIs as compared to miniplates?
Dr. Shah:
Miniplates offer greater success and stability than MSIs. [10] The greater success rate of the miniplates can be attributed to their higher primary stability which in-turn comes from the fact that a miniplate connects two or more MSIs.
However, the placement of miniplates is more invasive. A surgical flap needs to be raised and two surgeries are requiredone for its placement and one for its removal. Since multiple screws are required, their cost is higher as compared to MSIs. Miniplates are usually not placed in primary or mixed dentition patients due to their potential for damage to the teeth. On the other hand, MSI’s are comparatively less expensive and offer more options with placement locations.
In my personal opinion, miniplates are best reserved for patients with severe skeletal discrepancies such as skeletal Class III malocclusions. De Clerck et al have reported several studies showing successful implementation of miniplates for correction of skeletal Class III malocclusions with midface deficiency. [11, 12]
Editor:
Where does the success rate of MSIs stand today? What factors can help improve this success rate for the clinicians?
Dr. Shah:
The success rate of MSIs has steadily improved over the years due to the availability of increased knowledge and research. MSI success rate was reported to be more than 75% in 2008. [13] In 2009, a systematic review of MSIs based on 19 studies reported success rates greater than 80% if mobile and displaced implants were considered as successful. [14] A meta-analysis performed on the failure rates and associated risk factors of orthodontic MSIs in 2012 reported an overall success rate of 86.5%. [15].
As we continue to gather more critical information through further research in this field, we will be able to accomplish even higher success rate. From my personal experience, an appropriate selection of the placement site along with a thorough insertion protocol are some of the factors that can help the clinicians improve their success rate.
Editor:
Do these MSIs remain stable throughout the course of orthodontic treatment? What is the latest research on this?
Dr. Shah:
It was first reported by Liou et al that MSIs do not remain stationary under orthodontic forces. [16] Since then a number of studies have reported that MSIs do not remain in the same exact position during treatment but they do remain stable. A systematic review of mini-implant displacement under orthodontic loading showed that significant primary displacement ( immediate displacement straight after loading) was detected (6.4–24.4 mm) for orthodontic forces ranging from 0.5–2.5 N. [17] The mean secondary displacement (displacement over the treatment time) ranged from 0-2.7 mm for all MSIs.
Majority of studies done on this topic have confirmed that MSIs provide good anchorage quality during orthodontic treatment. However, clinicians can anticipate some displacement of MSI in the direction of force over time. Therefore, it would be prudent to evaluate proximity of adjacent vital structures such as teeth, nerves, and blood vessels before insertion of MSIs.
References
- Shah AH, Behrents RG, Kim KB, Kyung HM, Buschang PH (2012) Effects of screw and host factors on insertion torque and pullout strength. Angle Orthod82:603.
- Motoyoshi M, Uemura M, Ono A, Okazaki K, Shigeeda T, et al. (2010) Factors affecting the long-term stability of orthodontic mini-implants. Am J OrthodDentofacialOrthop137:e1–5.
- Ren Y, Maltha JC, Kuijpers-Jagtman AM (2003) Optimum force magnitude for orthodontic tooth movement: a systematic literature review. Angle Orthod73:86–92.
- Proffit W (2007) Contemporary Orthodontics. 4th ed. St Louis, Mo: Mosby.
- Lim SA, Cha JY, Hwang CJ (2008) Insertion torque of orthodontic miniscrews according to changes in shape, diameter and length. Angle Orthod78:234-240
- Morarend C, Qian F, Marshall SD, Southard KA, Grosland NM, et al. (2009) Effect of screw diameter on orthodontic skeletal anchorage. Am J OrthodDentofacialOrthop 136:224.
- DeCoster TA, Heetderks DB, Downey DJ, Ferries JS, Jones W (1990) Optimizing bone screw pullout force. J Orthop Trauma 4:169–174.
- Huja SS, Litsky AS, Beck FM, Johnson KA, Larsen PE (2005) Pullout strength of monocortical screws placed in the maxillae and mandibles of dogs. Am J OrthodDentofacialOrthop127:307–313.
- Friberg B, Sennerby L, Grondahl K, Bergström C, Bäck T, et al. (1999) On cutting torque measurements during implant placement: a 3year clinical prospective study. Clin Implant Dent Relat Res 1:75–83.
- Chen YJ, Chang HH, Huang CY, Hung HC, Lai EH, et al. (2007) A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res18:768.
- De Clerck H, Cevidanes L, Baccetti T (2010) Dentofacialeffects of bone anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J OrthodDentofacialOrthop138: 577.
- De Clerck HJ, Cornelis MA, Cevidanes LH, Heymann GC, Tulloch CJ (2009) Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral MaxillofacSurg67:2123.
- Buschang PH, Carrillo R, Ozenbaugh B, Rossouw PE (2008) Survey of AAO members on miniscrew usage. J ClinOrthod42: 513.
- Reynders R, Ronchi L, Bipat S (2009) Mini-implants in orthodontics: a systematic review of the literature. Am J OrthodDentofacialOrthop135:e1-19.
- Papageorgiou SN, Zogakis IP, Papadopoulos MA (2012) Failure rates and associated risk factors of orthodontic miniscrew implants: a meta-analysis. Am J OrthodDentofacialOrthop142:577-595.
- Liou EJ, Pai BC, Lin JC (2004) Do miniscrews remain stationary under orthodontic forces? Am J OrthodDentofacialOrthop126: 42.
- Nienkemper M, Handschel J, Drescher D (2014) Systematic review of mini-implant displacement under orthodontic loading. Int J Oral Sci6:1-6.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences