Role of Orthodontist in Obstructive Sleep Apnea - An Orthodontic Review
Luv Agarwal and Ankit Gupta
DOI10.21767/2469-2980.100027
Department of Orthodontics and Dentofacial Orthopedics, Saraswati Dental College and Hospital, Haridwar, Uttrakhand 249401, India
- *Corresponding Author:
- Luv Agarwal
Department of Orthodontics and Dentofacial Orthopedics
Saraswati Dental College and Hospital, Haridwar
Uttrakhand 249401, India
Tel: 9758571324
Fax: 9758571324
E-mail: luvagarwal789@gmail.com
Received date: June 27, 2016; Accepted date: August 18, 2016 ; Published date: August 25, 2016
Citation: Agarwal L, Gupta A. Role of Orthodontist in Obstructive Sleep Apnea An Orthodontic Review. J Orthod Endod. 2016, 2:3. doi: 10.4172/2469-2980.100027
Abstract
Obstructive sleep apnea (OSA) is a common sleep associated breathing disorder with profound effects on the health and quality of life of individuals suffering from it. Orthodontists should be well aware of the symptoms of this disorder and competent enough to recognize its signs and symptoms. Orthodontics is well suited for treatment of OSA patients due to their expertise and knowledge regarding growth and development of oro-facial and dento-facial structures as well as orthopedic, orthodontic and surgical correction of the jaws and other supporting tissues. The aim of this article is to provide an outlook to the essential role of orthodontists in the treatment of this serious disease.
Keywords
Obstructive sleep apnea; Orthodontics; Sleep; Snoring
Introduction
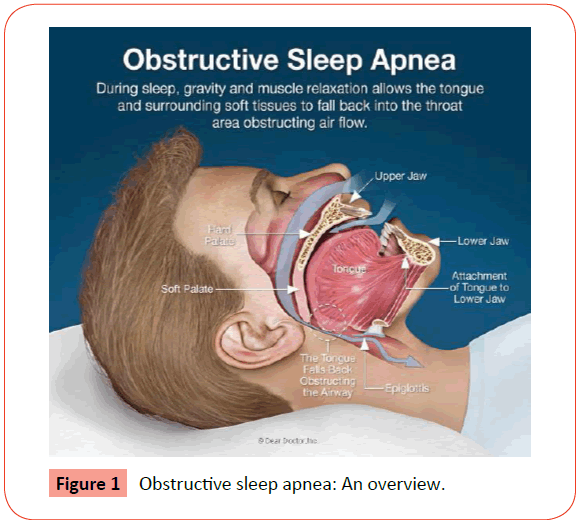
Obstructive sleep apnea (OSA) is a sleep-associated disorder of breathing with a reduction or complete airflow obstruction despite an ongoing effort by patient for breathing. It usually occurs during sleep, muscles undergoes relaxation and causes collapse of the soft tissues present in the back of the throat which leads to upper airway blockage (Figure 1). Consequently, there are partial and complete pauses in breathing that last at least 10 seconds during sleep. Then, blood oxygen saturation, with oxygen levels decreases abruptly and falls 50% or more in severe cases. The brain shows response when there is less oxygen and alerts the body which causes a brief arousal from sleep. This restores normal pattern of breathing. This pattern can occur hundred times in one night. This results a fragmentation in sleep quality and produces an excessive sleepiness during daytime [1,2]. Chronic persistent sleeping is a common symptom which prevails throughout the life and caused by interplay between a variety of factors including sleep-related loss of muscle tone in the tissues, large tonsils, large tongue, and anatomical obstruction of air passages, a retro gnathic mandible, alcohol, obesity, sedatives and allergic medications. Since sound of snoring is a key symptom of obstructive sleep apnea, it has become a medical concern [3].
In sleep study monitoring, the frequency of apneas and hypopneas per hour of sleep (apnea-hypopnea index [AHI]) is the key measure to define and stratify the severity of OSA, although inherent limitations to this metric include not taking into consideration degree of accompanying hypoxia, length of respiratory events, etc. AHI levels of 5, 15 and 30 have been used as cut-points to define mild moderate and severe OSA, respectively. Apnea can be distinguished as obstructive vs. central based upon presence or absence of thoracoabdominal effort [4,5].
Many studies have revealed an association between OSA severity and other common causes of increased mortality such as hypertension, stroke, coronary artery disease, and occupational, as well as automobile accidents. For this reason, OSA has been increasingly recognized as a major public health issue imposing great economic burden, thereby mandating early recognition and treatment [6-10].
Prevalence
OSA can occur in any age group, but prevalence increases between middle and older age. OSA with resulting daytime sleepiness occurs in at least 4% of men and 2% of women. About 24% of men and 9% of women have the breathing symptoms of OSA with or without daytime sleepiness. About 80% to 90% of adults with OSA remain undiagnosed. OSA occurs in about 2% of children and is most common at preschool ages [11-14].
Pathophysiology of Obstructive Sleep Apnea
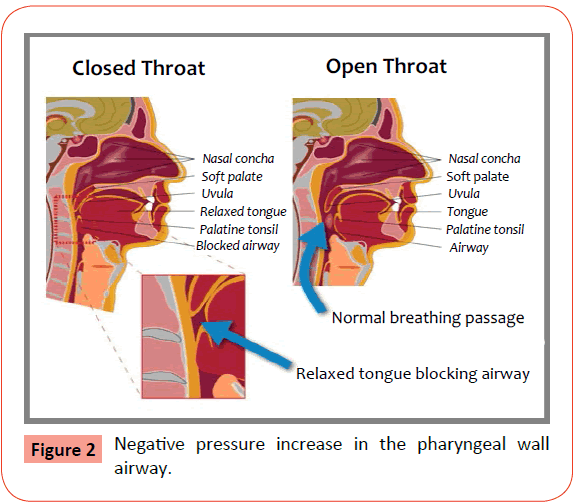
It has been considered that individuals with OSA have impairment in function of genioglossus muscle, which is a muscle of tongue. This causes the prolapse of the tongue against the posterior pharyngeal wall when there is inspiratory effort during sleep. Pharyngeal wall invaginates and airway occludes during sleep [15-18]. Obstruction in nasal air flow increases air flow resistance, which in turn increases effort for inspiration and increases negative pressure in the pharyngeal wall airway (Figure 2). This suction increases the chances of pharyngeal airway collapse [19-21].
Predisposing Factors
They are summarized in Table 1 [22-25].
| S.No. | Predisposing factors of OSAHS |
|---|---|
| 1 | Obesity |
| 2 | Presence of structural abnormalities that causes upper airway obstruction |
| 3 | Increasing age |
| 4 | Male gender |
| 5 | Smoking and alcohol consumption |
| 6 | Sedatives |
| 7 | Retrognathic mandible |
| 8 | Adenoids |
| 9 | Micrognathia |
| 10 | Enlarged tonsils |
| 11 | Enlarged tongue |
Table 1: Predisposing factors of OSAHS.
Symptoms of Obstructive Sleep Apnea
They are summarized in Table 2 [26-29].
| S.No. | Symptoms of OSAHS |
|---|---|
| 1 | Snoring |
| 2 | Apneic pauses ie..choking, gasping, snoring during the night |
| 3 | Restless sleep and increased body movements |
| 4 | Bruxism (nocturnal tooth grinding) |
| 5 | Nocturnal and daytime enuresis |
| 6 | Neck hyper extension |
| 7 | Growth failure restriction |
| 8 | Mouth breathing, due to dryness in mouth |
| 9 | Chronic nasal congestion |
| 10 | Walking during sleep |
| 11 | Obesity |
| 12 | Mouth breathing, due to dryness in mouth |
| 13 | Fatigue |
| 14 | Mood changes; irritabitility, frustration, impatience, depression, anxiety |
| 15 | Aggression and hyperactivity |
| 16 | Poor school performance |
| 17 | Poor concentration, and distraction |
| 18 | Infraorbital venous congestion |
Table 2: Symptoms of OSAHS
Features of Obstructive Sleep Apnea
They are summarized in Table 3 [30].
| S.No. | Features of OSAHS |
|---|---|
| 1 | Excessive daytime sleepiness |
| 2 | Impairment in concentration |
| 3 | Snoring |
| 4 | Disturbed sleep |
| 5 | Choking episodes during sleep |
| 6 | Apneas |
| 7 | Personality changes |
| 8 | Nocturia |
| 9 | Decreased libido |
Table 3: Features of OSAHS
Effects of Obstructive Sleep Apnea
They are summarized in Table 4 [31].
| S.No. | Effects of OSAHS |
|---|---|
| 1 | Fluctuations in oxygen levels |
| 2 | Increased heart rate |
| 3 | Chronic elevation in daytime blood pressure |
| 4 | Increased chances of stroke |
| 5 | Heart disease |
| 6 | Impairment in glucose tolerance and insulin resistance |
| 7 | Impaired concentration |
| 8 | Mood changes |
| 9 | Increased motor vehicle accidents |
| 10 | Disturbed sleep of the bed partner |
Table 4: Effects of OSAHS.
Diagnosis of Obstructive Sleep Apnea
The frequency of pauses in breathing on an hourly basis is used for assessment of the severity of the obstructive sleep apnea hypopnea syndrome (OSAHS) and it is called the apnea/hypopnea index (AHI) or the respiratory disturbance index (RDI). It is the one most commonly used [32].
OSAHS may be subdivided into three categories degrees of breathing abnormality, on the basis of AHI (Table 5) [33].
| S.No. | Forms of OSAHS | AHI Score |
|---|---|---|
| 1 | Mild | AHI 5-14/hr |
| 2 | Moderate | AHI 15-30/hr |
| 3 | Severe | AHI >30/hr |
| 4 | Very severe | AHI >40/hr |
Table 5: Forms of OSAHS.
Subjective assessment of sleepiness
Individuals with this disorder may present with non-specific symptoms such as poor concentration, irritability, personality changes and family problems. The patient should be asked the following questions:
• Are you falling asleep regularly against your will?
• Are you often feeling sleepy while driving?
• Are you having difficulty while working?
• Is surgery for snoring being performed?
The Epworth Sleepiness Scale (ESS) is a validated method used to assess the probability of falling asleep. The score subdivide the patients clinically into 4 categories (Table 6) [34].
| S.No. | Types of Sleepiness | ESS Score |
|---|---|---|
| 1 | Normal range | ESS <11 |
| 2 | mild subjective daytime sleepiness | ESS =11 |
| 3 | moderate subjective daytime sleepiness | ESS =16 |
| 4 | Severe subjective daytime sleepiness | ESS >18 |
Table 6: Epworth Sleepiness Scale (ESS).
Objective assessment of sleepiness
The Multiple Sleep Latency Test (MSLT) is used to measure the time to fall asleep (using EEG criteria). This is performed in a dark room on at least four separate occasions across the day. This period of time is called as sleep latency.
Physical examination
• Weight and height are noted at the first clinic visit. Changes in height and weight are observed at all subsequent visits as approx 50% of patients with OSAHS are obese (BMI >30 kg/m2).
• Circumference of neck are measured as patients with OSAHS often have increased neck circumference >17 (43 cm).
• Visually inspect for retrognathic mandible.
• Assess patency of nasal airway.
• Upper airway obstruction is assessed using indirect laryngoscopy if possible.
• Inspect the tongue for macroglossia.
• Assess dentition for the presence or absence of teeth.
• Assess pharynx for size of tonsil, appearance of uvula and size of lumen.
• Measure blood pressure.
• Perform respiratory, cardiovascular and neurological examination for detection of any disease such as cor pulmonale, deformity in chest wall and myopathies.
• Observe the possibility of hypothyroidism, acromegaly and thyroid function tests should be indicated [35-38].
Tools Used in Diagnosis of Obstructive Sleep Apnea
Polysomnography (PSG)
Polysomnography records patterns of sleeping and breathing together. PSG is performed overnight at a sleep centre with the help of a technician and a standard PSG typically consists of EEG, electromyogram, electro-oculogram, respiratory airflow, thoraco-abdominal movement and oxygen saturation tracings (oximetry).
Polysomnography requires about 30-60 min set up time before sleep and about 30 minutes detachment time in the morning. Staff should be present for at least ten hours overnight to perform and monitor this test [39-41].
Oximetry
Cheap recording pulse oximeters are readily available; therefore oximetry is used as the first screening tool for OSAHS. These are spectrophometric devices that are used for the detection and calculation of the differential absorption of light by presence of oxygenated and deoxygenated haemoglobin in blood. This is a method for detection of the blood oxygen saturation [42].
Treatment of Obstructive Sleep APNEA
Treatment options can be broadly divided into [43]:
1. Behavioral interventions
2. Non-surgical options
3. Surgical options
Behavioral interventions
Since patients with obstructive sleep apnea are obese, therefore patients should be advised to undergo weight reduction therapy as it improves symptoms of OSAHS and other related disorders. Smokers should be advised to stop smoking for general health.
Alcohol should not be used and drugs and sleeping tablets should be avoided as this may decrease airway dilator function and worsen OSAHS. Positional therapy is for patients who suffer from mild OSA. Patients should be advised from sleeping on their backs and head of the bed is raised to reduce symptoms [44].
Non-surgical interventions
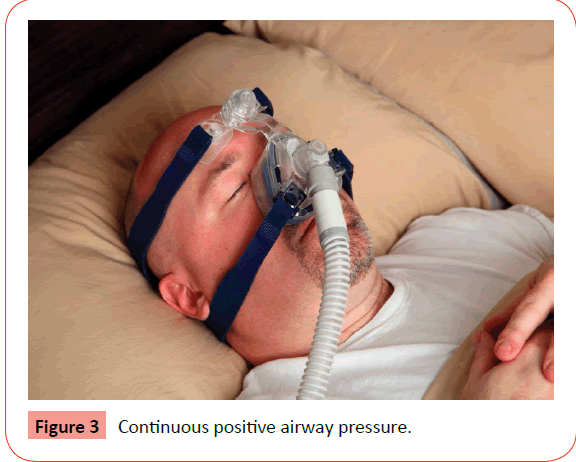
Continuous positive airway pressure (CPAP): CPAP is the treatment option for moderate to severe cases of OSA. A continuous positive airway pressure machine is a new device with a mask that fits snugly over the nose of patient. It transmits a continuous flow of air and keeps the throat open throughout the night (Figure 3).
Continuous positive airway pressure (CPAP) functions like a pneumatic splint and keeps the airway patent during sleep breathing. It works by means of a flow generator that delivers positive pressure through air tube to a nasal mask worn by the patient. This generation of airflow keeps the airway open and prevents pauses in breathing and restores normal oxygen levels. Newer CPAP devices are quite small, light and available with different mask sizes to achieve a good fit [45,46]. Major side effects of CPAP are significant epistaxis, paranasal sinusitis but they are rare [47,48].
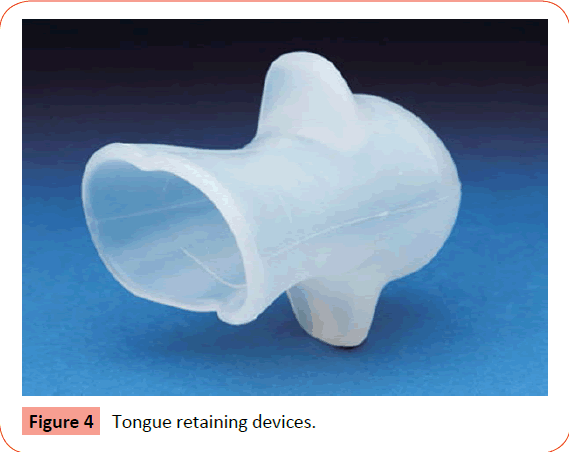
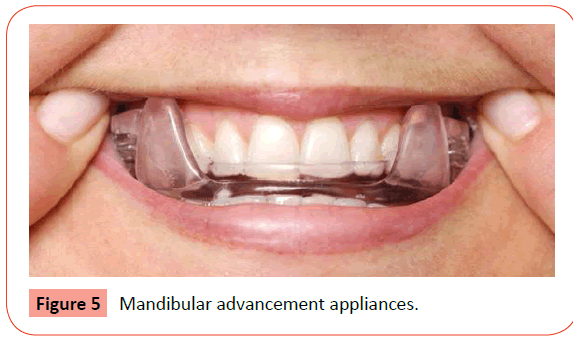
Oral appliance therapy: Orthodontic appliances should be fabricated in a way that it can be worn by the patient either in a permanent or removable manner depending upon the condition of the patient. These appliances bring the mandible and tongue forward, opens up the lower pharynx and allows continuous breathing during sleep [49,50]. Examples are tongue retaining devices (TRD) and mandibular advancement appliances (MAA) (Figures 4 and 5).
• Indications: 1) Patients with snoring or mild OSA who do not respond for treatment with behavioral measures. 2) Patients with moderate to severe OSA who refuse treatment with nasal CPAP. 3) Patients who are not appropriate for tonsillectomy, adenoidectomy, and tracheostomy.
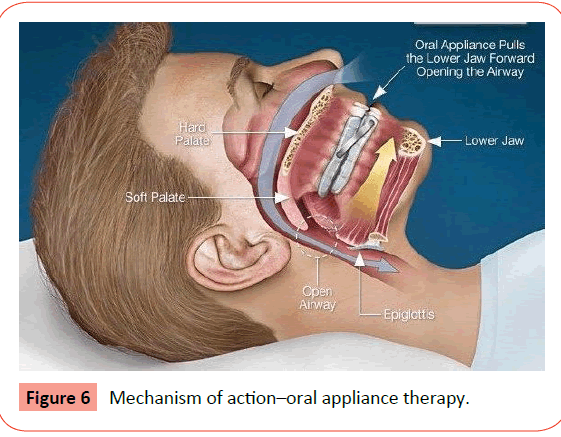
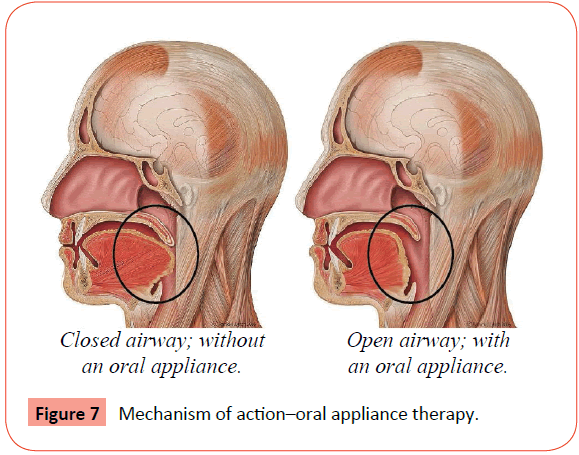
• Mechanism of action: Oral appliances are used only during sleep which repositions the lower jaw, tongue, soft palate or uvula and maintains an open and unobstructed airway. It protrudes the mandible and tongue forwards and prevents upper airway collapse during sleep (Figures 6 and 7).
• Advantage of Oral appliances
• Significant reduction in breathing pauses
• Improvement of airflow for some patient with apnea
• Reduction in the snoring and
• High compliance level as compared to CPAP
• Disadvantages of oral appliances: Reciprocal forces are generated on the teeth and jaw by mandibular advancement splints which results in dry mouth, gum soreness, salivation, tooth pain, headaches, and TMJ problems [51,52].
Surgical interventions
Surgery is considered when noninvasive therapy such as CPAP and oral appliances has been not successful. It is done in a situation when there is any deformity in anatomic structure that can be later on corrected to eliminate the breathing problems. It addresses the problem by reduction of tissue from the soft palate, uvula, tonsils, adenoids or tongue [53].
Many different surgical approaches have been used in the treatment of OSAHS.
Uvulopalatopharyngoplasty (UPPP): It is the reconstruction of the throat by resection of posterior margins of the soft palate and unwanted mucosa present on the pharyngeal walls [54].
Adenotonsillectomy: It is the surgical removal of the tonsils and adenoids and it is the most common treatment option for children with OSA.
Tracheostomy: Tracheostomy was the first surgical treatment for OSAHS and bypasses the obstruction completely [55,56].
Other surgical techniques
a) Bariatric (weight reducing) surgery: Weight influences the severity of OSAHS and weight loss is an effective treatment for OSAHS in some patients [57].
b) Nasal surgery: Nasal surgery reduces nasal airflow resistance and reduces pressure and improves compliance with nasal CPAP [58].
Consequences of untreated OSAHS
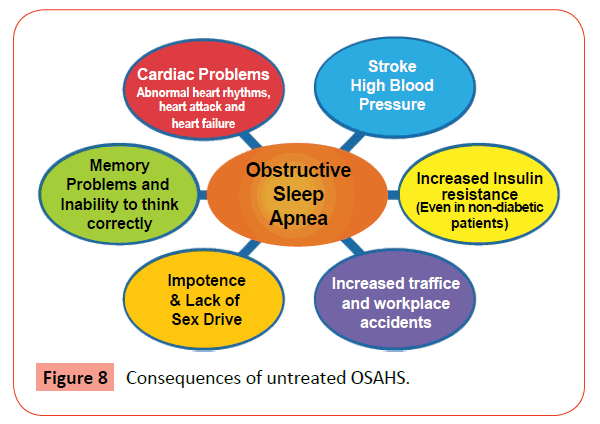
Obstructive sleep apnea negatively impacts quality of life and is also associated with a number of adverse safety and health consequences including cardiovascular disease and motor vehicle crashes. Short habitual sleep duration can result in excessive daytime sleepiness and reduced neurocognitive function. Sleep loss may have long-term health consequences and may lead to premature death, cardiovascular disease, and the development of diabetes. Patients may also experience impaired concentration due to tiredness, increased irritability, depression and mood changes. There is an increased risk of high blood pressure and may have a slightly increased risk of angina, heart attacks and strokes (Figures 8 and 9) [59-62].
Conclusion
The effects of untreated sleep apnea on daily activities are multiple and it includes excessive daytime sleepiness, impaired cognitive function, mood elevations and personality changes. It is also related with a reduction in quality of life and there can be adverse changes on others such as impaired relationships between spouses and partners. Symptoms of sleepiness sleep apnea are observed and these disorders need to be treated urgently. Orthodontists should play an active role in screening of patients for this disease and advise oral appliance therapy, if needed.
References
- Bliwise DL, Pascualy RA (1984) Sleep-related respiratory disturbance in elderly persons. ComprTher 10: 8-14.
- Guilleminault C (1985) Obstructive sleep apnea. The clinical syndrome and historical perspective. Med Clin North Am 69: 1187-1203.
- Gottlieb DJ, Whitney CW, Bonekat WH, Iber C, James GD, et al. (1999) Relation of sleepiness to respiratory disturbance index, the Sleep Heart Health Study. Am J RespirCrit Care Med 159: 502-507.
- American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22: 667-689.
- Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D,et al. (2005) Practice parameters for the indications for polysomnography and related procedures, an update for 2005. Sleep 28: 499-521.
- Young T, Peppard P, Palta M, Hla KM, Finn L, et al. (1997) Population-based study of sleep-disordered breathing as a risk factor for hypertension. Arch Intern Med 157: 1746-1752.
- Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, et al. (2001) Sleep-disordered breathing and cardiovascular disease, cross-sectional results of the Sleep Heart Health Study. Am J RespirCrit Care Med 163: 19-25.
- Meisinger C, Heier M, Lowel H, Schneider A, Doring A (2007) Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population, the MONICA/KORA Augsburg cohort study. Sleep 30: 1121-1127
- Lindberg E, Carter N, Gislason T, Janson C (2001) Role of snoring and daytime sleepiness in occupational accidents. Am J RespirCrit Care Med 164: 2031-2035.
- Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J (1999) The association between sleep apnea and the risk of traffic accidents, Cooperative Group Burgos-Santander. N Engl J Med 340: 847-851.
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, et al. (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328: 1230-1235.
- Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, et al. (2001) Prevalence of sleep-disordered breathing in women: effects of gender. Am J RespirCrit Care Med 163: 608-613.
- Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A (1998) Effects of age on sleep apnea in men: I. Prevalence and severity. Am J RespirCrit Care Med 157: 144-148.
- Bearpark H, Elliott L, Grunstein R, Cullen S, Schneider H, et al. (1995) Snoring and sleep apnea. A population study in Australian men. Am J RespirCrit Care Med 151: 1459-1465.
- Cistulli PA, Sullivan CE (1994) Pathophysiology of sleepapnea. In:Saunders NA, Sullivan C (eds.), Sleep and breathing, Newyor, NY: Marcel Dekkerpp: 405-448.
- Mathur R, Mortimore IL, Jan MA, Douglas NJ (1995) Effect of breathing, pressure and posture on palatoglossal and genioglossal tone. ClinSci (Lond) 89: 441-445.
- Isono S, Remmers JE, Tanaka A, Sho Y, Sato J, et al. (1997) Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J ApplPhysiol (1985) 82: 1319-1326.
- Schwartz AR, Gold AR, Schubert N, Stryzak A, Wise RA, et al. (1991) Effect of weight loss on upper airway collapsibility in obstructive sleep apnea. Am Rev Respir Dis 144: 494-498.
- Schwartz AR, Smith PL, Wise RA, Gold AR, Permutt S (1988) Induction of upper airway occlusion in sleeping individuals with subatmospheric nasal pressure. J ApplPhysiol 64: 535-542.
- Schwab RJ (2003) Pro: sleep apnea is an anatomic disorder. Am J RespirCrit Care Med 168: 270-271.
- Katz I, Stradling J, Slutsky AS, Zamel N, Hoffstein V (1990) Do patients with obstructive sleep apneahave thick necks? Am Rev Respir Dis 141: 1228-1231.
- Ulfberg J, Carter N, Talbäck M, Edling C (1996) Headache, snoring and sleep apnoea. J Neurol 243: 621-625.
- Martin SE, Mathur R, Marshall I, Douglas NJ (1997) The effect of age, sex, obesity and posture on upper airway size. EurRespir J 10: 2087-2090.
- Rowley JA, Aboussouan LS, Badr MS (2000) The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep 23: 929-938.
- Young T, Shahar E, Nieto FJ, Redline S, Newman AB, et al. (2002) Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med 162: 893-900.
- Bailey DR (2001) Oral evaluation and upper airway anatomy associated with snoring and obstructive sleep apnea. Dent Clin North Am 45: 715-32.
- Puvanendran K, Goh KL (1999) From snoring to sleep apnea in a Singapore population. Sleep Res Online 2: 11-14.
- Tami TA, Duncan HJ, Pfleger M (1998) Identification of obstructive sleep apnea in patients who snore. Laryngoscope 108: 508-513.
- Beutler LE, Ware JC, Karacan I, Thornby JI (1981) Differentiating psychological characteristics of patients with sleep apnea and narcolepsy. Sleep 4: 39-47.
- Issa FG, Sullivan CE (1982) Alcohol, snoring and sleep apnea. J NeurolNeurosurg Psychiatry 45: 353-359.
- Shneerson J, Wright J (2002) Lifestyle modification for obstructive sleep apnoea (Cochrane Review). In: The Cochrane Library, Oxford: Update Software.
- Moran WB, Orr WC (1985) Diagnosis and management of obstructive sleep apnea. Part II Arch Otolaryngol 111: 650-658.
- Dillon JE, Blunden S, Ruzicka DL, Guire KE, Champine D, et al. (2007) DSM-IV diagnoses and obstructive sleep apnea in children before and 1 year after adenotonsillectomy. J Am Acad Child Adolesc Psychiatry 46: 1425-1436.
- Johns MW (1993) Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth Sleepiness Scale. Chest 103: 30-36.
- Viner S, Szalai JP, Hoffstein V (1991) Are history and physical examination a good screening test for sleep apnea? Ann Intern Med 115: 356-359.
- Maislin G, Pack AI, Kribbs NB, Smith PL, Schwartz AR, et al. (1995) A survey screen for prediction of apnea. Sleep 18: 158-166.
- Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP (1993) Using the BerlinQuestionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131: 485-491.
- Kirby SD, Eng P, Danter W, George CF, Francovic T, et al. (1999) Neural network prediction of obstructive sleep apnea from clinical criteria. Chest 116: 409-415.
- Dixon JB, Schachter LM, O'Brien PE (2003) Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Chest 123: 1134-1141.
- Bornstein SK (1982) Respiration during sleep polysomnography. Addision -Wesley pp:183.
- Gastaut H, Tassinari CA, Duron B (1965) Polygraphic study of diurnal and nocturnal (hypnic and respiratory) episodal manifestations of Pickwick syndrome. Rev Neurol (Paris) 112: 568-579.
- Vazquez JC, Tsai WH, Flemons WW, Masuda A, Brant R, Hajduk E, et al. (2000) Automated analysis of digital oximetry in the diagnosis of obstructive sleep apneoa. Thorax 55: 302-307.
- Cistulli PA, Grunstein RR (2005) Medical devices for the diagnosis and treatment of obstructive Sleep Apnea. Expert Rev Medical Dev 2: 749-763.
- Smith PL, Gold AR, Meyers DA, Haponik EF, Bleecker ER (1985) Weight loss in mildly to moderately obese patients with obstructive sleep apnea. Ann Intern Med 103: 850-855.
- Weaver TE, Chasens ER (2007) Continuous positive airway pressure treatment for sleep apnea in older adults. Sleep Med Rev 11: 99-111.
- Mc Ardle N, Devereux G(1999) Long term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J RespirCrit Care Med 159: 1108-1114.
- Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, et al. (2007) Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning.Sleep 30: 711-719.
- Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT (2003) Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea, results of a meta-analysis.Arch Intern Med 163: 565-571.
- Lim J, Lasserson TJ, Fleetham J, Wright J (2006) Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev 25.
- Ferguson KA, Rogers (2006) Oral appliance for snoring and obstructive sleep apnea, review. Sleep 29: 244-262.
- Ng ATm,Gotsopoulos H(2003) Effect of oral appliance theraphy on upper airway collapsibility in obstructive sleep apnea. Am J RespirCrit Care Med 168: 238-241.
- Lowe AA (1999) Oral appliance for the treatment of snoring and obstructive sleep apnea. J Can Dent Assoc 65: 571-574.
- Sundaram S, Bridgman SA, Lim J, Lasserson TJ (2005) Surgery for obstructive sleep apnoea. Cochrane Database Syst Rev 19.
- Mortimore IL, Bradley PA, Murray JA, Douglas NJ (1996) Uvulopalatopharyngoplasty may compromise nasal CPAP therapy in sleep apnea syndrome. Am J RespirCrit Care Med 154: 1759-1762.
- Conradt R, Hochban W, Brandenburg U, Heitmann J, Peter JH (1997) Long-term follow-up after surgical treatment of obstructive sleep apnoea by maxillomandibular advancement. EurRespir J 10: 123-128.
- Sher AE (1995) Update on upper airway surgery for obstructive sleep apnea. CurrOpinPulm Med 1: 504-511.
- Charuzi I, Lavie P, Peiser J, Peled R (1992) Bariatric surgery in morbidly obese sleep apnea patients, short- and long-term follow-up. Am J ClinNutr 55: 594S-596S.
- Redline S, Adams N, Strauss ME, Roebuck T, Winters M (1998) Improvement of mild sleep-disordered breathing with CPAP compared with conservative therapy. Am J RespirCrit Care Med 157: 858-865.
- George CF (2001) Reduction in motor vehicle collisions following treatment of sleep apnoea with nasal CPAP. Thorax 56: 508-512.
- Young T, Blustein J, Finn L, Palta M (1997) Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults.Sleep 20: 608-613.
- Briones B, Adams N, Strauss M, Rosenberg C, Whalen C, et al. (1996) Relationship between sleepiness and general health status. Sleep 19: 583-588.
- Yang EH, Hla KM, McHorney CA, Havighurst T, Badr MS (2000) Sleep apnea and quality of life. Sleep 23: 535-541.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences