Internal Validation of Subjective Bayesian Model of The Occurrence of Alveolar Osteitis Cases, Generated by Expert in Kinshasa Hospital/DRC
Muyembi MP, Sekele JP, Kashiama B, Bobe P, Kalala EM, Nyimi Bushabu F, Dzaringa T, Tshilela M, Duan Feng F, Munyanga S and Mantshumba MA
DOI10.21767/2469-2980.100026
1Department of Stomatology, University of Kinshasa, Affiliated Hospital of Kinshasa University, Kinshasa, D. R. Congo
2Department of Medical and Food Anthropology, University of Kinshasa, Administrative and Political, Kinshasa, D. R. Congo
3Department of Oral and Maxillofacial Surgery, Second Affiliated Hospital of Jiamusi University, Jiamusi, China
4Department of Statistics, School of Public Health, University of Kinshasa, Kinshasa, D. R. Congo
- *Corresponding Author:
- Muinaminayi Pierre Muyembi
Internal Validation of Subjective Bayesian
Model of The Occurrence of Alveolar
Osteitis Cases, Generated by Expert in
Kinshasa Hospital/DRC.
Tel: 00243819072550
E-mail: pierremuyembim@gmail.com
Received date: June 25, 2016; Accepted date: July 26, 2016; Published date: July 29, 2016
Citation: Muyembi MP, Sekele JP, Kashiama B, et al. Internal Validation of Subjective Bayesian Model of The Occurrence of Alveolar Osteitis Cases, Generated by Expert in Kinshasa Hospital/DRC. J Orthod Endod. 2016, 2:2. doi: 10.21767/2469-2980.100026
Abstract
Objective: To valid an Internal Model Subjective of Bayer by the case of alveolar osteitis generated by the Experts.
Methods: The qualitative method was carried out under form of integration group, with had eight experts. The selection criteria of experts were to be a professor at the faculty of Dental medicine, a master's degree in oral surgery, dentistry, periodontology, prosthesis and to be dental doctor with more than 20 years of occupation. Elaboration of SBM was carried out by three steps such as determination of a prior probability of quotient (APRIQ), determination of the likelihood ratio (LHR) and Determination of a posteriori probability quotient (APPQ. And SBM was validated in three stages: determination of the agreement degree of intra and inter experts; of Cut off point (COP) and Internal validation. The agreement degree of intra and inter expert was determined by kappa statistics.
Results: Seven risks factors such as F1=bad oral and dental hygiene, F2=Systemic diseases, F3=pre-existent infections, F4=Preoperative Infection, F5=lack of asepsis, F6=unexperienced practitioner and F7=post-operative infection was identified. A prior probability of quotient was 0.21. Likelihood ratio (LHR) of 7 independents factors are LHR=F1=3; F2=1.5; F3=4; F4=1.5; F5=1.3; F6=1.5 and F7=3 and LHR=F11=0.28; F2=0.25; F3=0.16; F4=0.4; F5=0.75; F6=0.33 and F7=0.14.
Conclusion: The Poor oral hygiene LHR3; post-operative infections LHR3, preoperative infections LHR4, were the most important identified factors predictive of occurrence of AO in our 8 dental hospital of D. R. Congo/Kinshasa city. The corrected of these three factors can contribute to reduce the frequency of that pathology in Kinshasa population.
Keywords
Alveolar osteitis; Internal validation; Subjective bayer’s model
Introduction
An operations of oral surgery is relate primarily on the teeth, soft tissue and bone. Despite the advance of restorative dentistry and prosthetic rehabilitation techniques as well as periodontics, the dental extractions still a very common surgical practice in Africa [1,2].
In certain conditions, despite the perfect knowledge of the practitioner and mastering of the surgical plan, the surgical operations can be delicate and difficult to predict some complications during or after surgery. In the postoperative, the most frequent complications of dental extraction are inflammatory or infectious such as alveolar osteitis (AO), which includes the dry and suppurative alveolitis [3-5].
This study was initiated to identify 7 groups’ factors of occurrence of AO by a mathematical model of Bayer, which is based on the opinions of experts who use the qualitative data [6-8]. Clinical interest will be to help the clinicians use a mathematical model for the 7 predictive factors of AO such as non-modified factors (age and gender) and modified factors (poor oral hygiene, systematic diseases, infections, aseptic technique, lack of practitioner, the postoperative infections [5,9-12]. However, it is possible to prevent the occurrence of AO in patients with the modified risk factors [3,5,12].
In some development countries, the dental extractions are often followed by postoperative complications, which result as a high morbidity of the patients [1,2,13,14]. However, in Democratic Republic of Congo, no study found from the literature have been initiated on the AO by using a mathematical model. From 2011, Muyembi et al. [11] conducted a descriptive prospective and preventive study of AO in the Affiliated Hospital of Kinshasa University and the result of pattern occurrence of AO found was 13.3%. This is a sign that the AO relates are not only concern to the less educated person, but also in all class or category of the persons such as university workers, graduates or students of Kinshasa University, with morbid consequences that flow from it [11,14].
Thus, view the increase frequency postoperative of AO and its consequences of economic and social disability of the patient due days work in the development countries and view the lacking information and training of the population of the Democratic Republic of the Congo for the good oral health, due to the decrease of dental surgeons in our country (one surgeons/4.865 population in Kinshasa Capital where there is a large population, estimated at 10,000,000 people); we have been asked to conduct a qualitative study on the determinants of the occurrence of AO in the eight major Dental hospitals of Kinshasa city [14-19].
The results of the mathematical model built will used for an elaboration of tree clinical decision, and will help us to reflect the prediction software of AO. Then, on the basis of this model, we will do an algorithm treatment of all oral diseases post-dental extraction.
This study aims was to identify the occurrence factors of AO in Kinshasa population treated at 8 major dental Hospital and will make the recommendations for to improve the management of dental extraction of numerous service of stomatology in Democratic Republic of Congo in general, and particular to Kinshasa Capital.
Materials and Methods
This study used a qualitative method under form as a nominal group, which is based on Bayesian statistics and adapted from work of Gustafson [20,21]. The choice of this method is justified by the fact that these statistics are help to use the opinions, the subjective elements provided by experts for to generate the statistics on the basis of the evidence [8,22,23]. The qualitative method was carried out under form of integration group, with had eight experts. It has helped to identify the factor can establish the occurrence of AO in patients who dental extractions were mad from 8 dental clinics hospital of Kinshasa (D. R. Congo).
It was conducted by six steps: (1) Selection of experts; (2) Interview of experts (search of a consensus on the definition of variables and elaboration a provisional list of predictors factors); (3) Training of experts; (4) Establishment list of predictive factors; (5) Regrouping of independent factors and (6) Elaboration model. The selection criteria of experts were to be a professor at the faculty of Dental medicine, a master's degree in oral surgery, dentistry, periodontology, prosthesis and to be dental doctor with more than 20 years of occupation. All have the skills and knowledge of AO, and be available during the period of our study. Interview of experts by Brainstorming followed by technique of nominal group, have been help resulted an elaboration of provisional list factors of AO; used for an elaboration of the Subjective Bayesian model (SBM).
Elaboration of SBM was carried out by three steps: determination of a prior probability of quotient (APRIQ), determination of the likelihood ratio (LHR) and Determination of a posteriori probability quotient (APPQ)
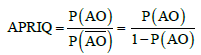
a) The prior probability of quotient (APRIQ) was established from an arithmetic mean of the different estimations of expert on the probability of occurrence of AO). P(AO) compared with the probability of non-occurrence of AO  .
.
The probability of AO; P (AO) was obtained by asking this question to experts: “On 10 patients treated in your department, how much have been developed the AO?” The probability of occurrence of AO, P(AO) was obtained by the sum of the frequencies estimated by 8 experts. The probability of non-occurrence of AO,  have been deducted according to the law of the probability distribution,
have been deducted according to the law of the probability distribution,  =1- P(AO).
=1- P(AO).
b) The determination of the likelihood ratio (LHR) for each independent factor identified by experts (Fi, i = 1, …., F7 and (Fi, i = 1, ……, 7), likelihood ratio (LHR ) help to establish an impact of each factor on the studied event. LHR > 1, the factor increased the occurrence of AO; LHR < 1, the factor decreases the occurrence of AO, and negative if LHR = 1
c) Determination of a posteriori probability quotient (APPQ): The APPQ is obtained by multiplying the different likelihood ratios by the a priori probability quotient (APRIQ). APPQ = LHR × APRIQ.
d) Probability occurrence of O.A:  and SBM was validated in three stages: 1) Determination of the agreement degree of intra and inter experts; 2) Determination of Cut off point (COP); 3) Internal validation.
and SBM was validated in three stages: 1) Determination of the agreement degree of intra and inter experts; 2) Determination of Cut off point (COP); 3) Internal validation.
Establishment of an agreement degree of intra and inter experts was performed by 8 experts who each built 5 cases hypothesis, either 40 cases of AO, with the presence of this or that factors can contributed on the occurrence of AO at twice individually. And determination of occurrence of AO in the plenary. The agreement degree of intra and inter expert was determined by kappa statistics using this formula:
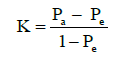
Pa = Agreement probability expected
Po = Agreement probability observed
K = A value between 0 and 1. If K < 0.4 low agreement; 0.4 ≤ K 0.6 means agreement; 0.6 ≤ K < 0.8 good agreement; K ≥ 0.8 excellent agreement
This internal validation of the subjective Bayesian model (SMB) will be determined from the case of alveolar osteitis on which the experts shall reached consensus on the occurrence or non-occurrence of AO. Then parameters such as sensitivity (Sy), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV) and overall efficiency value (OEV) will be evaluated [10].
Determination of COP will be calculate by these parameters for each value between 0.1 and 0.9. The COP was determined and corresponds to the value of SBM that has a higher sensitivity and greater specificity.
Results
Factors identified
Eight experts were included in study and the unmodifiable factors such as gender and age (10-80 years) wasn’t been taken account. Seven independent modified factors and exclusive were obtained by the technique of Nominal groups techniques are shown in Table 1.
| Factors (F) | Regroupment |
|---|---|
| F1: Bad oral and dental hygiene | • Poor or bad oral hygiene state • Smoker • Environmental factors, economic andsocio-geographical |
| F2: Systemic diseases leading to the deficiencyof immunity | • Immune deficiency (anemia, diabetes, AIDS, Avitaminosis) |
| F3:Pre-existent infections | • Apical periodontitis acute with abscess • Apical periodontitis chronic with granuloma • Periodontal infection of vicinity • Hot tooth extraction • The aero-anaerobic microorganisms • Multifactorial • Healthy factors |
| F4: Preoperative Infection | • Alveolar curettage • Alveolar infection • Pre-operative infection by bacteria |
| F5: Lack of asepsis | • No asepsis ( operator-materials) |
| F6: Unexperienced practitioner | • Traumatic extraction • Mandible localization of extraction • Extraction Difficulty • Residuals fragments (bone, dental, tartars • Third mandibular molars or impacted teeth • Bad used xylocaine anesthesia with vasoconstrictor • Singular extraction than numerous • Vascular trauma • Bad design of mucoperiosteal flap • Bad suture post-operative |
| F7: Post-operative infection | • Intensive rinsing the wound • Move out the alveolar clot • Postoperative Mouth wash by Nacl solution • Infection of postoperative wound by bacteria ,biofilm |
Table 1: Independent 7 factors and exclusive obtained by nominal group technique.
Elaboration of SBM
Determination of a prior probability of quotient (APRIQ): From clinical experience of experts, an average number of patients treated in 8 dental clinics hospitals and developed an AO on 10 cases were established. The mean number of patients who did not developed an AO was deduced. The occurrence probability of AO in patient P (AO) was estimated at 0.175 and its complementary probability P (OA ̅) was deduced at 0.825.
The value of AFRIQ was less than 1, thus prediction of experts showed that a patient has less chance to develop an AO.
The determination of the likelihood ratio (LHR) of independents factors: Different likelihoods ration of 7 factors generated by the experts are: LHR = F1 = 3; F2 = 1.5; F3 = 4; F4 = 1.5; F5 = 1.3; F6 = 1.5 and F7 = 3; LHR = F1 = 0.28; F2 = 0.25; F3 = 0.16; F4 = 0.4; F5 = 0.75; F6
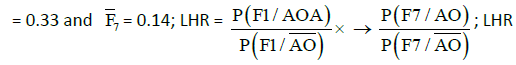
= 3 × 1.5 × 4 × 1.5 × 1.3 × 1.5 × 3 = 157.9 ( impact development of AO is positive).
Determination of a posteriori probability quotient (APPQ): APPQ = LHR × APRIQ =157.9 × 0.21 = 33.159.
Determination of probability for to develop or not an O.A:
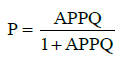
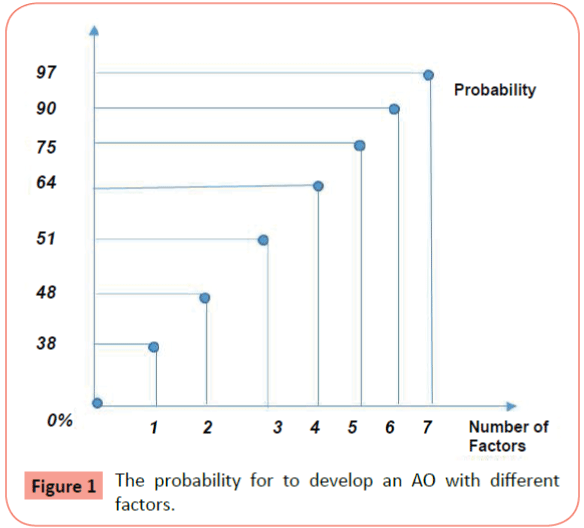
The mathematic model showed that, the probability for to develop an AO with: 7 factors = 0.97 = 97%; 6 factors = 0.90 = 90%; 5 factors = 0.75 = 75%; 4 factors = 0.64 = 64%; 3 factors = 0.51 = 51%; 2 factors = 0.48 = 48%; 1 factor = 0.38 = 38%; 0 facto = 0% (Figure 1).
Validation of model: Application of SBM elaborated for to analyze the case of AO designed by the experts, showed that the kappa statistics was acceptable: higher than 0.4, indicating a likewise reason of expert. Comparison results of AO provided by 8 experts with or without factors showed that le SBM predicts the occurrence of AO in 30 cases (75%), and the non-occurrence of AO in 10 cases (25%). Kappa value was greater than 0.4 was accepted in consensus by the experts. Therefore, the group is considered to be homogeneous and the arithmetic mean of estimated probabilities can be used to assess the SBM.
Determination of criteria of COP (cut off point): The high value of COP from different opinions of the experts was for Sy (93.8%), Sp (89.5%), PPV (88.2%), NPV (94.4%) and OEV (19.4%) obtained at point 0.5.
Validation of internal SBM: Application of SBM, with the values of COP at 0.5, compared to the consensus of experts showed that SBM predicts an occurrence of AO in seven cases and no occurrence of AO in the same cases confirmed by consensus of expert. The model has a good validity and performance of test of Sy 81.3%, Sp 89.5% PPV 86.5%, NPV 85% and OEV 85.7%.
Discussion
Occurrence of AO in patients treated from 8 Dental clinics was determined by SBM with combination of seven factors such as F3: pre-operative infection (LHR = 4), F1: poor oral dental hygiene (LHR = 3 ), F7: postoperative infection (LHR = 3), F2: systemic diseases with low immunity (LHR = 1.5 ), F6: inexperience of practitioner (LHR = 1.5) F4: Per operative infection (LHR = 1.5), F5 asepsis (LHR = 1.3) [5,12].
The likelihood ratio (LHR) of SBM value (157.9), showed that these factors had an important positive impact on the occurrence of AO; APRIQ value (0.21) inferior to 1, shows that the patients had less chance for to develop an AO. All seven risks factors of AO found in the literature have been restraint by the SBM like an impact positive of AO occurrence [2,3,5,9,10,12,24].
Once all seven risks factors are present in the patients, the probability for to develop an AO according to the SBM is more with 97 percent and that is a high risk of the patient. But once only six factors, five, four, three and two factors are presents in the patients, the risk for to develop an AO is presented differently. However, the risk occurrence of AO is zero if no risk factor is present. The recent result are similar from others conclusions of some studies stipule that, an association of the factors, constitute a force in the occurrence of AO [2,3,5,9,12,24]. Then, the correct management of postoperative complication was contribute to reduce the occurrence of AO to 0.5% in the development countries [5,12].
Prevention treatment is the most priority for to reduce the occurrence of AO, because can help to detect at time the modified factors of AO and intervint by efficiently [2-4,11]. The main force of this study result an elaboration model that had grouped the numerous factors in only seven risks factors and that can render it simple usage.
In clinical situation, the sensitivity and the specificity are most often used because, the sensitivity for a damage such as AO will be based on the definition, on the characteristics and signs of this disease. In particular, it is not likely to vary from one hospital to another. The same rationale applies to the specificity because it is also based on the definition, characteristics and signs of the disease [9]. While the predictive values on the contrary, are functions of the respective proposals of patients and nonpatients in the population. These predictive values vary from one hospital to another for the same pathology; hence they are less used as evaluation parameters [9].
Limits of our study
• Different expert can produce a different a posteriori probability that can some time laid to a little low performance of SBM study.
• Was no objective measure of occurrence of AO. The occurrence was measured by opinions of experts from a consensus on the definition of occurrence and risks factors.
• We hope to have a large sample of cases of AO from numerous dental clinics than use in the study.
Conclusion
The SBM such as built can permit to calculate the probability occurrence of AO in the patients that a dental extraction will be indicated for the reason that the presence or absence of one or numerous risks factors identified by experts. The Poor oral hygiene LHR3; post-operative infections LHR3, preoperative infections LHR4, were the most important identified factors predictive of the occurrence of AO in our dental clinics of D. R. Congo/Kinshasa city.
The corrected of these three factors can contribute to reduce the frequency of that pathology in our population.
References
- AgodaP (2005) The dental extraction at the CHU in Lomé (Togo) about 981 patients from 1996 to 2001. Dév Et Sant 178: 6.
- Badiane C (200) Alvéolectonie first line-dental surgicalinterest. Dakar.
- Blondeau F (2007) The extraction of mandibularthirdmolars, postoperative complications and riskfactors. JADC73: 325a-325c.
- Bui CH (2003) Types, frequencies, and Riskfactors for complications afterthirdmolars extractions. AmAss Oral-Max-Surg2003: 1379-1389.
- Antonia KolokythasE(2010) Alveolarosteitis (OA), a comprehensivereview of concepts and controversies.Int J Dent 2010:249073
- Charles H, Hennekens (1998) Epidémiologie en médecine. Edition: Frison-Rochee.
- PewsneraD, Bleuerb JP, Bucherc HC, Battaglia DM, Jüni P, et al. (2001) On the path of intuition ? Bayes theorem and diagnosis in general practice.Partie I Forum Méd Suisse Nn3: 17.
- MafutaE, Mudipanu, MunyangaSM, Bwira EM (2014) Determinants of the success of incomegeneratingactivitiesmanaged by a person living with HIV in Kinshasa, DemocraticRepublic of the Congo: a glance of congoleseexperiences. Ann Afr Med 7: 3.
- Diouf A (2007) Oral biofilm and dental diseases. Antibiotiques SAS 2007: 181-188.
- Gassama Barry (2009) The first line alvéolectoni: surgicalinterest in about 101 cases. Revue du COSA-CMF 16: 44.
- Muyembi (2011) Preventing dental alveolitispostextractions the UniversityClinics of Kinshasa (DRC). Honorsthesis in Oral Surgery, Faculty of Medicine, Kinshasa.
- Nekson (2011) Factorsassociatedwith complications from the removal of thirdmolars: A cross-sectionalstudy.Méd Oral pathChir Buccal 16: E375-E380.
- RDC (2015) Ministry of Planning: Monograph Kinshasa. Avril 2005.
- OMS RDC (2014) Ministry of Public Health, USA places the healthsector. Rapport provisoire,April-June, 1998.
- UNDP (2014) United Nations Development Programme in the RDC. Province de Kinshasa.
- RDC (2014) Presidency of the Republic. DirectorHealthDevelopment Plan. PDDS 2006-2009.
- RDC (2014) Ministry of Public Health, General Secretariat. National healthdevelopment plan,PNDS, 2011-2015.
- OMS RDC (2014)Ministry of public health, national humanresourcesdevelopment for health. 2011-2015.
- UNDP (2014) UN programs for development, fightagainstpoverty Unit. Province de Kinshasa.
- GustafsonH, David H(1992) Systems to support healthpolycyanalysis. HealthAdministration Press, Chicago.
- Gustagson H, David H (1993) The construction, reliability, validit, application and impact of a quality Index for spychiatric, Emergencies. HealthServices Research28: 131-158.
- Lim SS, Vost, Vos T, Flaxman AD, Danaei G, Shibuya K, et al. (2016) A comparative Riskassessment of burden of disease and injuryattributable to 67 riskfactors and Risk factor clusters in 21 regions: 1990-2010. Lancet 380: 2224-2260.
- World HealthOrganization (2008) The global burden of disease 2004. Geneva.
- Engeland CG,Bosch JA, Cacioppo JT,Marucha PT (2006) MucosalWound Healing, The roles of Age et sex. ArchSurg 141: 1193-1197.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences