Root Fracture in Teeth with Cast Metal Retainers: Clinical Case Report
Raquel Tolentino*
Department of Odontology, Pontifical Catholic University of Minas Gerais, Belo Horizonte, Brazil
- *Corresponding Author:
- Raquel Tolentino
Department of Odontology,
Pontifical Catholic University of Minas Gerais, Belo Horizonte,
Brazil;
Email: clinica_tol@hotmail.com
Received: March 27, 2020, Manuscript No. ipjoe-20-3669; Editor assigned: March 30, 2020, PreQC No. ipjoe-20-3669; Reviewed: April 13, 2020, ipjoe-20-3669; Revised: June 28, 2022, QI No. ipjoe-20-3669; Manuscript No. ipjoe-20-3669; Published: 26-July-2022, DOI: 10.36648/2469-2980.2022.8.7.23
Citation: Tolentino R (2022) Root Fracture in Teeth with Cast Metal Retainers-Clinical Case Report. J Orthod Endod Vol: 8 No: 7:23.
Abstract
Intraradicular retainers are cylindrical or conical structures traditionally made of metal or fiberglass used in the root canal of endodontically treated teeth. They have been widely used in cases where the remaining coronal structure of the tooth is not sufficient to provide adequate support for the restorative material. Metal retainers have a much greater modulus of Elasticity (E) than the glass fibre. This was the factor pointed out as responsible for allowing greater resistance to fracture in the system due to the greater ability to withstand the load concentration before the deformation indicated in cases where high occlusal loads are present, such as patients with bruxism and absence of adequate occlusion.
Keywords
Intraradicular retainers; Elasticity; Glass fibre; Patients
Introduction
The absence of a remaining coronal structure is one of the conditions that still challenges the selection of the retainer. A review showed that the posts behave better when a remaining 2 mm coronal structure is present, providing the ferrule effect [1]. Thus, the present article consists of reporting the case of a patient with the left lateral incisor treated endodontically and with a metal intraradicular retainer and crown showing a root fracture, where it was necessary to perform a more invasive approach, performing the extraction of the element and after 3 months, the dental implant will be made [2]. The study aims to highlight the main differences between metallic and fiberglass intraradicular retainers, with a systematic approach in their main indications, advantages, limitations and flaws.
Case Study
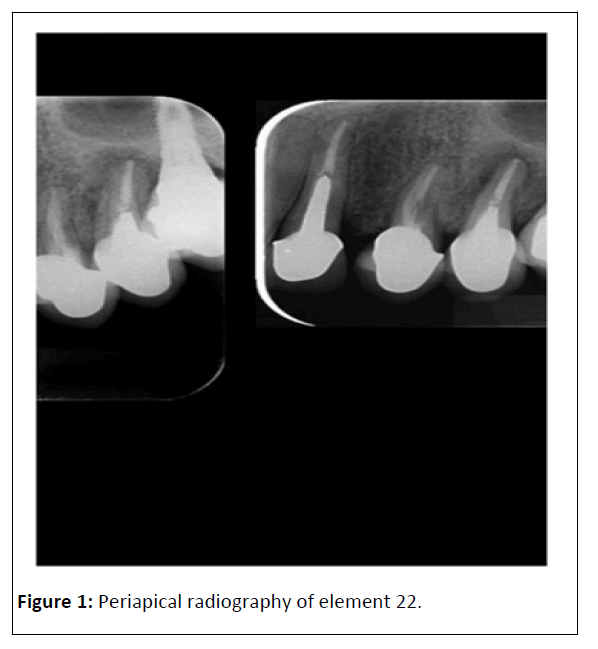
Patient M.A.O.S., leucoderma, 59 years old, male, attended a private clinic reporting: "I bit a hard food and I heard a snap in the teeth". During the clinical examination, the patient reported painful symptoms after the event. Then, a radiographic examination was performed (Figure 1).
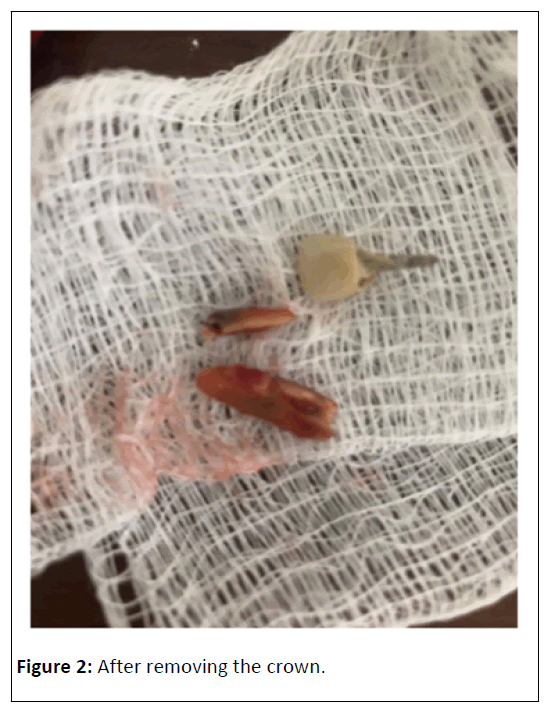
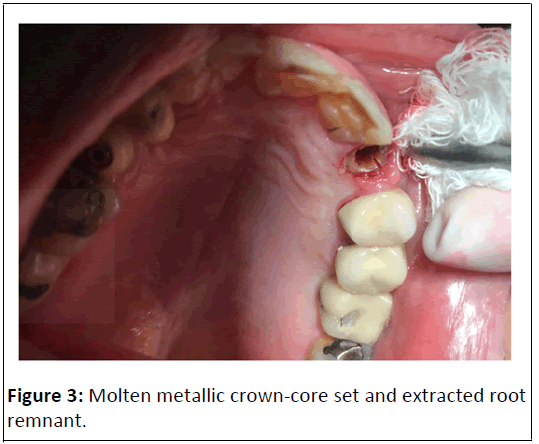
It was possible to observe that element 22 had previously received endodontic treatment, and a metallic intraradicular retainer and crown was made. The slightly lacerated root is a predisposing factor to a possible root fracture, especially in this tooth with a metal retainer [3]. Analyzing the radiography carefully, a vertical root fracture was detected in the distal region of the root of the dental element. As the fracture extended up to the middle third of the root, the treatment plan chosen was for atraumatic extraction of tooth 22, followed by a dental implant. Firstly, the crown and intraradicular retainer set was removed (Figure 2), and soon after removal, it was possible to see the vertical root fracture. Then, the removal of the fractured portion and tooth extraction were completed (Figure 3). Finally, the patient will use a temporary removable partial dentures for about 3 months, followed by a dental implant replacing the extracted element [4,5].
Discussion
Substantial loss of coronal tooth structure as a result of tooth decay, trauma and endodontic therapy can affect the overall strength of a tooth without pulp. Several studies have indicated that tooth strength is directly related to the rest of dentin [6]. Several materials have been used for the manufacture of intraradicular retainers. Metal alloys have been the material of choice for decades. However, several authors have reported that the use of an intraradicular retainer with a significantly higher elasticity module than dentin can create stresses at the cementinterfaces, with the possibilityinterfaces, with the possibility of post-separation or root fracture [7]. According to the current literature, teeth treated endodontically have a higher risk of fracture than vital teeth due to the decreased moisture content in dentin and, in most cases, compromise structural integrity.
For functional and aesthetic reasons, protesis of the type crown total, together with the retainer, are often recommended to improve crown retention [8,9]. The cast metal retainers technique has been advocated as the gold standard restoration for decades, but the traditional technique is time consuming and involves high laboratory and material costs. The introduction of prefabricated core systems and aesthetic core systems, such as ceramic reinforced with fiber and zirconia, significantly improved the results. In cases of complex oral rehabilitation; dentin, cement, abutment, retainer, crown and their interfaces can have varying concentrations of stress due to their different mechanical characteristics when the masticating forces are exerted [10]. It has been suggested that the material of the intraradicular retainer has an elasticity modulus similar to that of dentin (18.6 GPa) to distribute the applied forces evenly along the length of the column and the root.
Differences in the biomechanical behavior of teeth restored with prefabricated fiberglass and metallic retainers were observed. However, they show similarities regarding fracture resistance. Metal retainers are traditionally made of alloy with an elastic modulus much larger than that of dentinae and are responsible for supporting high chewing loads before defracturing. In addition, the metallic core is made in perfect juxtaposition with the dental structure, minimizing the thickness of the cement layer, also responsible for providing a high fracture load [11]. However, the placement of prefabricated cores also provides some benefits. For example, a specific drill for channel preparation, with the same shape and thickness as the fiberglass pin, provides a precise adaptation of the prefabricated core. The fiberglass pins are repackaged with composite resin directly into the root canal, ensuring juxtaposition. A thin layer of resin cement was identified as important to provide friction and pin retention [12].
The other main reason for the similarity in fracture resistance between the cores is the ferrule effect. Although the use of a prefabricated retainer should be less resistant than the metallic one, this study showed that the reinforcement provided by the intracanal relining is sufficient to promote similar fracture resistance when 2 mm of remaining coronal structure is present. The ferrule effect means that axial parallel to the dentin walls provide a protective effect, reducing the stress between the structure of the nucleus and the dental element, helping to better distribute the stress along the tooth structure after being surrounded by the crown [13]. In addition, studies have shown that metal cores under constant action of masticatory loads provide slow crack growth and adhesive failure of the retainer/ cement/dentin interface. After loose adhesion, more energy is transferred to the tooth structure causing the fracture. Prefabricated retainers led to less contact pressure, especially when the re-fiberglass pins were used [14]. This is explained by the fact that the fiberglass posts have flexural behavior similar to that of dentin, which minimizes stresses in the tooth structure and in the retainer/dentin interface. The greater contact pressure observed in the metallic core when compared to prefabricated posts can be attributed to the smaller contact area with dentin (pressure=force/area). Therefore, for metallic cores, the stresses are concentrated only at the core/dentin interface, while groups of prefabricated posts dissipate stress along the root canal.
Conclusion
Therefore, the use of a retainer glass fibre should be considered as a viable option for the rehabilitation of teeth with little coronal structure in daily clinical practice, to provide adequate retention to the coronal remnant of the tooth. As can be seen that the tooth had a dental clinical remnant with the possibility of making a retainer glass fibre. Among the failures of the retainer glass fibre, it can be considered that in the worst case it would de-stem due to inadequate preparation. Despite this, this fact does not delegitimize the wide usefulness of metal retainers in rehabilitation treatments, especially in teeth with little or no coronal remnant. In the clinical case in question, the lacerated root, the metal retainer and the excessive mechanical load were the main factors for the vertical root fracture to occur.
References
- Verissimo C, Junior PCS, Soares CJ, Noritomi PY, Santos-Filho PCF (2014) Effect of the crown, post, and remaining coronal dentin on the biomechanical behavior of endodontically treated maxillary central incisors. J Prosthet Dent 111: 234-246.
- Pereira JR, do Valle AL, Shiratori FK, Ghizoni JS, Bonfante EA (2014) The effect of post material on the characteristic strength of fatigued endodontically treated teeth. J Prosthet Dent 112: 1225-1230.
- Maroli A, Hoelcher KAL, Reginato VF, Spazzin AO, Caldas RA, et al. (2017) Biomechanical behavior of teeth without remaining coronal structure restored with different post designs and materials. Mater Sci Eng C 76: 839-844.
- Khaledi AAR, Sheykhian S, Khodaei A (2015) Evaluation of retention of two different cast post-core systems and fracture resistance of the restored teeth. J Dent 16: 121.
- A Alharbi F, Nathanson D, Morgano SM, Baba NZ (2014) Fracture resistance and failure mode of fatigued endodontically treated teeth restored with fiber‐reinforced resin posts and metallic posts in vitro. Dent Traumatol 30: 317-325.
- Aggarwal R, Gupta S, Tandan A, Gupta NK, Dwivedi R, et al. (2013) Comparative evaluation of fracture resistance of various post systems using different luting agents under tangential loading. J Oral Biol Craniofac Res 3: 63-67.
- Abduljabbar T, Sherfudhin H, AlSaleh SA, Al-Helal AA, Al-Orini SS, et al. (2012) Fracture resistance of three post and core systems in endodontically treated teeth restored with all-ceramic crowns. King Saud Univers J Dent Sci 3: 33-38.
- Pinto CL, Bhering CLB, de Oliveira GR, Maroli A, Reginato VF, et al. (2019) The influence of post system design and material on the biomechanical behavior of teeth with little remaining coronal structure. J Prosthodont 28: e350-e356.
- Bacchi A, Dos Santos MBF, Pimentel MJ, Caetano CR, Sinhoreti MAC, et al. (2013) Influence of post-thickness and material on the fracture strength of teeth with reduced coronal structure. J Conserv Dent 16: 139.
- Zhou L, Wang Q (2013) Comparison of fracture resistance between cast posts and fiber posts: A meta-analysis of literature. J Endodont 39: 11-15.
- Clavijo VGR, Reis JMDSN, Kabbach W, Oliveira Junior OBD, Andrade MFD (2009) Fracture strength of flared bovine roots restored with different intraradicular posts. J Appl Oral Sci 17: 574-578.
- Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M (2012) Ferrule effect: A literature review. J Endod 38: 11-19.
- Barcellos RR, Correia DPD, Farina AP, Mesquita MF, Ferraz CCR, et al. (2013) Fracture resistance of endodontically treated teeth restored with intra-radicular post: The effects of post system and dentine thickness. J Biomech 46: 2572-2577.
- Santos-Filho PCF, Verissimo C, Soares PV, Saltarelo RC, Soares CJ, et al. (2014) Influence of ferrule, post system, and length on biomechanical behavior of endodontically treated anterior teeth. J Endod 40: 119-123.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences